The UK has a long track record of promoting global sexual and reproductive health and rights (SRHR) both as an important donor and advocate. As a former architect of the Family Planning 2020 (FP2020) initiative, it has contributed to significant progress in addressing the unmet contraceptive needs of women and girls globally, and has played a crucial role in securing international support for SRHR within the global international development agenda.
But these gains, which the UK has been such a positive force in attaining, are at serious risk of stalling or even being reversed as a result of the UK Government’s decision to reduce official development assistance (ODA). In the midst of continuing challenges to health systems due to the global pandemic and rollback of women’s rights globally, the importance of increased UK support for SRHR cannot be overstated.
In this new report, the Royal College of Obstetricians and Gynaecologists (RCOG) makes the case for urgent reinvestment in global SRHR. Supporting women and girls to access their SRHR is not only the right thing to do; it is critical to achieving the UK’s objectives for international development. The recently published International Women and Girls Strategy 2023-2030 rightly recognises SRHR as a key priority for gender equality. The RCOG welcomes the ambitions of the Strategy as an opportunity for the UK to once again take up the mantle of global champion of SRHR, but seizing this opportunity is dependent on a UK commitment to provide dedicated and sufficient long-term funding.
To reprise its role as a leading advocate of SRHR globally and deliver on the ambitions of the Women and Girls Strategy, the RCOG recommends that the UK government:
1. Make the commitments of the Women and Girls Strategy a reality by increasing investment in SRHR:
- Restore ODA to 0.7% of gross national income (GNI) in 2024-25 and commit to 0.7% for the next 10 years.
- Ring-fence the equivalent of 0.5% GNI for expenditure on development assistance delivered outside the UK.
- Spend £500 million per year for the next three years in SRHR programming and supplies.
- Publish clear spending targets and timelines for SRHR and gender equality, including how it will deliver on its 2021 commitment to restoring funding for women and girls.
2. Strengthen the UK’s global advocacy on SRHR by investing in new and existing global partnerships and collaborations, particularly on stigmatised issues:
- Restore support to the United Nations Population Fund (UNFPA) core operating fund alongside existing commitments to its Supplies Partnership, to ensure future stability in global SRHR supply chains.
- Renew the UK’s commitment to the Family Planning 2030 (FP2030) initiative.
- Champion the integration of abortion care into sexual and reproductive health services through the Foreign Commonwealth and Development Office’s (FCDO) programmes and through national universal healthcare plans as part of health system strengthening efforts.
- Champion prioritisation of the gynaecological health needs of women and girls on the global health agenda, to influence the investment of other donors.
- Build on commitments to tackling female genital mutilation (FGM) by collaborating with medical bodies and colleges to create a global network of health workers to tackle rising medicalisation.
3. Ensure that the life-course approach of the Women and Girls Strategy is truly comprehensive by targeting investment in evidence-based, scalable interventions:
- Scale up self-management and telemedicine in settings where it can provide safe additional pathways to increase access to SRHR.
- Collect data and research on the scale of the burden of gynaecological disease across the life course for women and girls, to build a strong evidence base to support future investment.
- Integrate contraception services into maternal services, post-abortion care and childhood immunisation programmes.
- Strengthen human papillomavirus (HPV) immunisation programmes in low- and middle-income countries (LMICs).
- Develop and deliver high-quality, evidence-based fistula repair and emergency obstetric training.
4. Invest in task shifting and task sharing for health workers as part of commitments to strengthening health systems, to support the delivery of comprehensive and integrated SRHR services:
- Publish clear spending plans and timelines for health systems strengthening.
- Invest in training for non-specialist healthcare providers to diagnose, prevent and treat gynaecological disease at an early stage.
- Invest in training a wider range of providers and health facilities to support the expansion of abortion care provision.
- Invest in supporting task shifting for long-acting reversible contraception (LARC) to expand access where feasible.

RCOG training on gynaecological health in Dhaka, Bangladesh
RCOG training on gynaecological health in Dhaka, Bangladesh

The UK has long played a critical role in the promotion of global SRHR – not only as one of the largest donors to SRHR initiatives but as one of the most progressive global leaders and advocates for SRHR, and more recently bodily autonomy. However, in recent years, this exceptional track record has been undermined by cuts to international development.
Since November 2020, UK-funded SRHR programmes with proven impact have faced disruption and even closure, compounding existing challenges to global health due to the COVID-19 pandemic and a growing global backlash against SRHR. While the full impact of the cuts can only be estimated, there is no doubt that this decision and its fallout has seriously jeopardised the health and rights of women and girls across the world, as well as lessening the UK’s standing as a donor and advocate in the field of women’s rights and international development.
The moral obligation to support women and girls’ SRHR is clear: bodily autonomy is the foundation upon which women and girls can exercise their full rights. Within the wider context of a global rollback on rights, UK support for SRHR has never been more important. For governments and donors, it is also a development ‘best buy’. For every $1 invested in family planning and maternal health in low-income countries, $8.40 is accrued by averting unintended pregnancies and reducing the demand for and cost of maternal and other health services.2
Most of all, supporting women and girls to take control of their reproductive health is essential to achieving the UK’s international development objectives, in particular the ‘3 Es’ of its International Women and Girls Strategy 2023-2030: education; ending violence; and empowering women and girls and championing their health and rights. If women and girls are to be supported to stay in school, to pursue employment and have economic security, to fully participate in social and political life and make decisions about their own bodies, they must be supported to have access to SRHR.
The benefits of universal access to SRHR cannot be realised without long-term and comprehensive investment. Even before the COVID-19 pandemic, funding for sexual and reproductive healthcare had stagnated.3 It is estimated that from 2022 to 2030, low- and middle-income countries (LMICs) will need to spend an additional $79 billion to end unmet need for family planning and end preventable maternal deaths.2
In this report, the RCOG aims to highlight the historical successes of UK leadership and funding commitments to SRHR over the last decade, while also beginning to describe the scale of the damage wrought by the recent cuts to the UK’s ODA. It is illustrated by the testimonies of RCOG Fellows and Members working in women’s health around the world, as well as other health professionals and NGO workers who are experiencing the impact of cuts on the frontline. The report makes the case for an urgent review of UK overseas development spending, with a view to re-establishing previous levels of funding. It advocates for a comprehensive approach to investment in SRHR, shining a light on currently under-prioritised areas as well as best practice and innovative service delivery models for low-resource settings.

RCOG training on gynaecological health in Dinajpur, Bangladesh
RCOG training on gynaecological health in Dinajpur, Bangladesh
About the RCOG
The RCOG works to improve women’s healthcare across the world. The College is committed to developing the accessibility and quality of education, training and assessments for doctors wishing to specialise in obstetrics and gynaecology (O&G).
Founded in 1929, the RCOG has been transforming women’s healthcare for over 90 years. We are recognised nationally and overseas as a leader in women’s healthcare, enabling us to build incredible international partnerships. With this network and expertise, we are working to advance the science and practice of O&G globally.
Today, the RCOG has over 16,500 members worldwide. Healthcare professionals in the O&G specialty can access support throughout each stage of their career. The RCOG encourages all our members to pursue lifelong learning and development, offering cutting-edge training programmes and courses.
The Centre for Women’s Global Health (the Centre) works to deliver the RCOG’s global mission to improve girls’ and women’s sexual and reproductive health in LMICs. Our operational model places RCOG Fellows, Members, and the women they serve front and centre of all we do.
We draw on the RCOG’s gold standard training, guidance and clinical expertise to train healthcare professionals in essential skills and promote evidence-based clinical best practices in women’s health. The Centre works with the RCOG Policy and Public Affairs team to amplify the lessons and experiences of our members and partners, providing a platform for them to be heard in international advocacy spaces, to influence policy and practice reform and call for greater investment in SRHR globally.
A note on language and terminology
Within this document we use the terms woman and women’s health. However, it is important to acknowledge that it is not only women for whom it is necessary to access women’s health and reproductive services in order to maintain their gynaecological health and reproductive wellbeing. Gynaecological and obstetric services and delivery of care must therefore be appropriate, inclusive and sensitive to the needs of those individuals whose gender identity does not align with the sex they were assigned at birth.

The UK Government plays an important role in the advancement of SRHR globally. The first part of this paper highlights just a few examples of the UK’s achievements in this field over the last decade.
It is against the backdrop of the success of UK support that the impact of cuts to SRHR programmes since 2020 is then described in part two, illustrated by the testimonies of RCOG members, other health professionals and NGO workers on the frontline. Part three looks forward to the opportunities presented by recent UK international development strategies for restoring progress on SRHR and re-establishing the UK as a global champion of SRHR, and makes recommendations about how this can be achieved with sufficient and long-term investment.
1. UK support for global SRHR: Timeline 2012-2020
July 2012
The UK Government, together with the Bill & Melinda Gates Foundation, USAID and the UNFPA, launches the FP2020 initiative, a ground-breaking effort to deliver voluntary modern contraception to an additional 120 million women and girls in the world’s poorest countries by 2020.
The UK commits to spending an average of £180 million every year on family planning, enabling an additional 24 million women and girls to access family planning services, averting over 20 million unintended pregnancies and preventing around 42,000 maternal deaths.4
‘The health and rights of girls and women are front and centre of Britain’s aid programme. Being able to plan the size of her family is a fundamental right that we believe all women should have.’
– The Rt. Hon Andrew Mitchell, former Secretary of State for International Development (2012)5
September 2015
At the UN General Assembly, the UK plays a key role in securing a stand-alone goal on gender equality as part of the 2030 SDGs (SDG5), including targets on SRHR, early and forced marriage, and female genital mutilation, alongside a target for universal SRHR access as part of the goal for universal health coverage (SDG3).6
The UK is also a champion of the ‘leave no one behind’ principle, which commits to reducing the structural inequalities that leave individuals, families and communities marginalised and excluded from sustainable development, in order to deliver on the 2030 agenda.7
‘We believe that no one should face the indignity of extreme, absolute, chronic poverty, no one should be denied the opportunity to realise their full potential or to share in progress, no one should be unfairly burdened by disaster or a changing climate, and no one should have their interests systematically overlooked.’
– From ‘Leaving no one behind: Our promise’ (2015)8
July 2017
The UK Government co-hosts a further summit to revitalise commitments to reaching the FP2020 goals, raising an additional £1.9 billion in funding for reproductive health services and securing financial commitments from three new donor countries.9
The UK Government significantly reviews and increases its own commitment, pledging an additional £45 million towards family planning – a total of £225 million every year until 2022 – making it the largest bilateral donor within the initiative.10
Despite significant recent cuts to support for SRHR supplies, the UK has ultimately exceeded that commitment, spending an average of £246 million on family planning every year from 2017 to 2022.11
‘We know that family planning, from a development perspective, is one of the smartest and savviest tools that we have out there. And it’s a clear investment any country can make when it comes to poverty reduction.’
– The Rt. Hon Priti Patel, former Secretary of State for International Development (2017)12
March 2018
Following extensive consultation with civil society, the UK’s Department for International Development (DFID) publishes its Strategic Vision for Gender Equality (SVGE).13
The Vision commits to supporting universal SRHR as one of its five priorities for delivering gender equality, including action on sex and relationships education, family planning, safe abortion, and maternal and newborn health.
‘As we make hard-headed decisions on how to invest UK aid, we know that empowering women and girls gives us the best return for our investment.’
– The Rt. Hon Penny Mordaunt, former Secretary of State for International Development (2018)14
The SVGE is progressive in its recognition that only a systemic approach, which addresses the root causes of gender inequality, can ensure the outcomes imagined by the UN SDGs (an approach that has unfortunately not been carried through to the FCDO’s15 Women and Girls Strategy). It commits to mainstreaming gender equality throughout the UK’s development programme and to joining up action across the life cycle and across the multiple areas of violence against women, girls’ education, economic and political empowerment and SRHR, to ensure that no girl or woman is left behind.
November 2018
The UK announces £200 million funding for a flagship comprehensive SRHR programme – Women’s Integrated Sexual Health (WISH) – to deliver voluntary family planning services and reproductive health and rights across 27 countries in Africa and Asia.
This investment represents 20% of the UK’s financial commitment to the FP2020 initiative.
Despite subsequent cuts to funding, the programme goes on to avert 12.8 million unintended pregnancies, 4.3 million unsafe abortions and over 22,000 maternal deaths.16
April 2019
In keeping with its commitment to leave no one behind, the UK Government announces £21 million for ACCESS – a new programme that aims to develop and test innovative approaches for supporting marginalised populations, particularly those affected by conflict and crisis, to access SRHR.17, 18
The programme is intended to be implemented over five years in four countries (Lebanon, Mozambique, Nepal and Uganda) where natural disasters and political instability have created complex and challenging environments for the delivery of universal SRHR.
However, due to the decision to cut overseas spending, the programme is closed shortly after it begins. Before its closure it is already producing results, including providing evidence to support the permanent introduction of self-management for medical abortion in Nepal.19
November 2019
At the 2019 Nairobi Summit of the International Conference on Population and Development (ICPD), the UK Government endorses the Guttmacher-Lancet Commission’s definition of comprehensive SRHR.20
The definition explicitly states that sexual and reproductive health is not possible without sexual and reproductive rights. The UK Government also endorses the associated recommended package of services, which includes less commonly provided interventions such as safe abortion care, comprehensive sexuality education, the prevention and management of reproductive cancers, and counselling for gender-based violence.21
The UK Government also announces £600 million for a new reproductive health commodity programme. This is intended to support 20 million women and girls to access family planning, five million more than the UK’s previous reproductive health supplies programme, by improving the availability, quality and supply of family planning and medicines.22 It includes a multi-year commitment of £425 million to the UNFPA Supplies Partnership, the world’s largest provider of donated contraceptives. This commitment is the largest financial partnership in UNFPA’s history.23






1. UK support for global SRHR: Timeline 2012-2020
July 2012
The UK Government launches the FP2020 initiative
The UK Government, together with the Bill & Melinda Gates Foundation, USAID and UNFPA, launches the FP2020 initiative, a ground-breaking effort to deliver voluntary modern contraception to an additional 120 million women and girls in the world’s poorest countries by 2020.
The UK commits to spending an average of £180 million every year on family planning, enabling an additional 24 million women and girls to access family planning services, averting over 20 million unintended pregnancies and preventing around 42,000 maternal deaths.4
‘The health and rights of girls and women are front and centre of Britain’s aid programme. Being able to plan the size of her family is a fundamental right that we believe all women should have.’
– The Rt. Hon Andrew Mitchell, former Secretary of State for International Development (2012)5
September 2015
The UK successfully lobbies for a gender equality UN Sustainable Development Goal (SDG) and for a commitment to ‘leave no one behind’
At the UN General Assembly, the UK plays a key role in securing a stand-alone goal on gender equality as part of the 2030 SDGs (SDG5), including targets on SRHR, early and forced marriage, and female genital mutilation, alongside a target for universal SRHR access as part of the goal for universal health coverage (SDG3).6
The UK is also a champion of the ‘leave no one behind’ principle, which commits to reducing the structural inequalities that leave individuals, families and communities marginalised and excluded from sustainable development, in order to deliver on the 2030 agenda.7
‘We believe that no one should face the indignity of extreme, absolute, chronic poverty, no one should be denied the opportunity to realise their full potential or to share in progress, no one should be unfairly burdened by disaster or a changing climate, and no one should have their interests systematically overlooked.’
– From ‘Leaving no one behind: Our promise’ (2015)8
July 2017
The UK co-hosts a further summit to revitalise commitments to FP2020
The UK Government co-hosts a further summit to revitalise commitments to reaching the FP2020 goals, raising an additional £1.9 billion in funding for reproductive health services and securing financial commitments from three new donor countries.9
The UK Government significantly reviews and increases its own commitment, pledging an additional £45 million towards family planning – a total of £225 million every year until 2022 – making it the largest bilateral donor within the initiative.10
Despite significant recent cuts to support for SRHR supplies, the UK has ultimately exceeded that commitment, spending an average of £246 million on family planning every year from 2017 to 2022.11
‘We know that family planning, from a development perspective, is one of the smartest and savviest tools that we have out there. And it’s a clear investment any country can make when it comes to poverty reduction.’
– The Rt. Hon Priti Patel, former Secretary of State for International Development (2017)12
March 2018
The UK publishes its ‘Strategic Vision for Gender Equality’
Following extensive consultation with civil society, the UK’s Department for International Development (DFID) publishes its Strategic Vision for Gender Equality (SVGE).13
The Vision commits to supporting universal SRHR as one of its five priorities for delivering gender equality, including action on sex and relationships education, family planning, safe abortion, and maternal and newborn health.
‘As we make hard-headed decisions on how to invest UK aid, we know that empowering women and girls gives us the best return for our investment.’
– The Rt. Hon Penny Mordaunt, former Secretary of State for International Development (2018)14
The SVGE is progressive in its recognition that only a systemic approach, which addresses the root causes of gender inequality, can ensure the outcomes imagined by the UN SDGs (an approach that has unfortunately not been carried through to the FCDO’s15 Women and Girls Strategy). It commits to mainstreaming gender equality throughout the UK’s development programme and to joining up action across the life cycle and across the multiple areas of violence against women, girls’ education, economic and political empowerment and SRHR, to ensure that no girl or woman is left behind.
November 2018
The UK launches WISH, its flagship SRHR programme
The UK announces £200 million funding for a flagship comprehensive SRHR programme – Women’s Integrated Sexual Health (WISH) – to deliver voluntary family planning services and reproductive health and rights across 27 countries in Africa and Asia.
This investment represents 20% of the UK’s financial commitment to the FP2020 initiative.
Despite subsequent cuts to funding, the programme goes on to avert 12.8 million unintended pregnancies, 4.3 million unsafe abortions and over 22,000 maternal deaths.16
April 2019
The UK announces a new programme for improving the provision of SRHR to marginalised groups
In keeping with its commitment to leave no one behind, the UK Government announces £21 million for ACCESS – a new programme that aims to develop and test innovative approaches for supporting marginalised populations, particularly those affected by conflict and crisis, to access SRHR.17, 18
The programme is intended to be implemented over five years in four countries (Lebanon, Mozambique, Nepal and Uganda) where natural disasters and political instability have created complex and challenging environments for the delivery of universal SRHR.
However, due to the decision to cut overseas spending, the programme is closed shortly after it begins. Before its closure it is already producing results, including providing evidence to support the permanent introduction of self-management for medical abortion in Nepal.19
November 2019
The UK endorses comprehensive SRHR and announces a new Reproductive Health Supplies programme
At the 2019 Nairobi Summit of the International Conference on Population and Development (ICPD), the UK Government endorses the Guttmacher-Lancet Commission’s definition of comprehensive SRHR.20
The definition explicitly states that sexual and reproductive health is not possible without sexual and reproductive rights. The UK Government also endorses the associated recommended package of services, which includes less commonly provided interventions such as safe abortion care, comprehensive sexuality education, the prevention and management of reproductive cancers, and counselling for gender-based violence.21
The UK Government also announces £600 million for a new reproductive health commodity programme. This is intended to support 20 million women and girls to access family planning, five million more than the UK’s previous reproductive health supplies programme, by improving the availability, quality and supply of family planning and medicines.22 It includes a multi-year commitment of £425 million to the UNFPA Supplies Partnership, the world’s largest provider of donated contraceptives. This commitment is the largest financial partnership in UNFPA’s history.23

2. The COVID-19 pandemic
The COVID-19 pandemic caused serious disruption to access to SRHR services, particularly in low-income countries, as resources and personnel were diverted to the public health emergency. Supply chain disruptions led to product shortages, while movement restrictions and fears about exposure discouraged many people from visiting health facilities.
![A quote from Dr Huma Sheikh, an obstetrician and gynaecologist based in Pakistan. A quote beneath says: All forces were aligned towards [addressing the COVID-19 pandemic]… even the medical students were busy. So the reproductive health and family planning sectors were left unattended.](./assets/n313l5ExIr/dr-huma-quote-1-900x1250.png)
The disproportionate impact of the pandemic on women and girls24 reduced access to sexual and reproductive health (SRH) services, leading to an increased incidence of negative SRH outcomes. In some countries, school closures resulted in an increased risk and incidence of pregnancy among adolescent girls,25 and there were heightened rates of domestic violence due to rising household economic insecurity and isolation.26
It is estimated that the pandemic disrupted contraceptive use for about 12 million women across LMICs, resulting in as many as 2.7 million unintended pregnancies in the first year,27 and that there were 1.5 million additional unsafe abortions in the first six months of the pandemic alone.28 Furthermore, the pandemic reduced access to the full scope of SRH care, particularly to already deprioritised SRHR interventions such as elective gynaecology and safe abortion care, despite the significant burden of morbidity and mortality caused by their absence.

3. Cuts to the UK official development assistance budget
Having played a critical role in the promotion of global SRHR for over a decade, in November 2020 the UK Government announced a temporary reduction in the UK’s ODA budget due to economic pressures caused by the pandemic.
The commitment was reduced from 0.7% of gross national income (GNI) to 0.5%,29 a cut of over £3,000 million (21.1%), on top of the existing drop in ODA spending due to the decrease in the size of the economy in 2020.30 The UK was the only G7 country to cut its development budget.31
Over the next few months, the UK Government made direct cuts to SRHR programmes, including support to UNFPA and the UK’s own SRHR programme, WISH. The UK’s ACCESS programme was closed after only a few months in operation, despite already showing good results. SRHR programmes were also indirectly affected by the end of other streams of funding for health, such as the Tropical Health and Education Trust (THET) managed Health Partnership Scheme,32 and by major cuts to flagship FCDO health sector programmes such as Saving Lives in Sierra Leone (SLiSL).33
United Nations Population Fund (UNFPA): Historically, the UK was the largest donor to UNFPA, the UN’s sexual and reproductive health agency, including to its Supplies Partnership. Between 2018 and 2021, UK funding is estimated to have averted 7.1 million unintended pregnancies, 2.1 million unsafe abortions and nearly 20,000 maternal deaths.
During 2021-22, nearly £150 million was cut from UK funding to UNFPA, including an 85% cut to the Supplies Partnership, meaning the UK fell to being only the 16th largest overall donor to the agency in 2021.
Although there has been a partial restoration of funding to the UNFPA Supplies Partnership, with a payment of £60 million for the 2022-23 financial year, support for the UNFPA’s core operating fund remains significantly reduced.
Sources: UNFPA – Donor contributions: United Kingdom of Great Britain and Northern Ireland;34 and Contribution from UNFPA to the International Development Committee’s inquiry into the FCDO’s approach to sexual and reproductive health35
![A photo of Dr Syeda Batool Mazhar, Obstetricican and Gynaecologist based in Islamabad, Pakistan. Beneath is a quote which says:We have definitely suffered [since the UK ODA cuts], especially with regard to the family planning programme. During the COVID times the funding was totally cut off. We had nothing to offer to the patient for contraception because it was just not available.](./assets/KK0eaxT0ZU/dr-syeda-900x1250.jpg)
It is important to note that the full extent of the cuts remains only partially understood, and this understanding relies largely on NGOs and other agencies sharing information and speaking out publicly. The most recent data provided by the UK Government shows that bilateral spending on SRHR decreased by over 50%, from £515 million in 2019 to £242 million in 2021.36 Countries and regions with the greatest need for SRHR funding and programmes are likely to have been hit the hardest: bilateral ODA allocation to Africa has fallen by 66% (from £2.27 billion in 2020 to £764 million in 2021-22).37

At a time when health services were already under enormous pressure due to the global pandemic, there is no doubt that the cuts to UK overseas development funding have had devastating consequences for women and girls. Indeed, the UK Government itself predicted this outcome in an FCDO Equalities Assessment undertaken in early 2021.38 Estimates by the Guttmacher Institute suggest that cuts to family planning in 2021-22 alone could directly result in 9.5 million fewer women and girls having access to modern methods of contraception, leading to 4.3 million more unintended pregnancies, 1.4 million more unsafe abortions and a possible 8,000 more avoidable maternal deaths.39

Within this broader picture, it is inevitable that the impact of the cuts has been disproportionately shouldered by the most marginalised groups and individuals – those with the greatest need, but who face the greatest barriers to accessing SRHR services.
![A quote from Professor Friday Okonofua,an Obstetrician and Gynaecologist based in Benin, Nigeria. A quote beneath says: We must consider these statistics [from the Guttmacher Institute’s research] in light of the hugely unequal access to healthcare in Nigeria: nearly 80% of health payments are out-of-pocket and the most marginalised [people] have long relied on donor-funded services. The loss of funding from the UK Government, previously a key supporter, will widen this dire gap in services.](./assets/f56bOydwIF/dr-friday-1-900x1250.jpg)
The Women’s Integrated Sexual Health (WISH) programme: WISH, the UK’s flagship SRHR programme, has also been subject to cuts. MSI Reproductive Choices, one of the programme’s two delivery partners, reports a 79% reduction in funding from 2019-20 to 2023-24. Cuts have led to the closure of service delivery in 13 countries, halving the programme’s global footprint. MSI has reported almost 8,000 fewer maternal deaths averted as a result of cuts, a drop of 87.5%, and over 850,000 fewer safe abortions, falling from 969,000 to 116,600, with the greatest reductions in Ethiopia and Mali. These statistics are even more shocking given that Mali is the 13th most dangerous country to give birth in, with a maternal mortality rate that is twice the global average. Beyond the numbers, the WISH programme’s delivery partners report that the reduction in funding has severely affected trust between clients and service providers. It has also damaged relationships between public service providers and national governments, pushing back progress on building long-term public sector SRH capacity and creating more space for opposition. They report having to make ‘difficult decisions about what and where we deliver’, with those with the greatest need, such as disabled women and girls, most likely to miss out.
Sources: Contribution from MSI Reproductive Choices40 and the International Planned Parenthood Federation41 to the International Development Committee’s inquiry into the FCDO’s approach to sexual and reproductive health; and Trends in Maternal Mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division42

4. Overseas development spending after the pandemic
Notwithstanding cuts to funding, the UK Government has not lost sight of the need to support SRHR around the world. In December 2021, the FCDO published the Ending Preventable Deaths of Mothers, Babies and Children by 2030 (EPD) approach paper, which committed to championing SRHR as part of its efforts towards reducing maternal and child mortality.43
In a joint paper, the FCDO also committed to strengthening health systems, including the health workforce, and promoting a rights-based approach to achieving universal health coverage.44 The UK also remains a strong and key advocate for SRHR in multilateral spaces, co-leading a statement at the UN General Assembly in October 2022 on the importance of respecting the bodily autonomy and SRHR of women and girls,45 as well as providing £3.45 million to UNFPA to support women and girls affected by the Russian invasion of Ukraine.46
While these are welcome interventions, there remains a gap between the UK Government’s stated political ambitions and the reality of ongoing cuts to ODA. Neither the EPD paper nor the paper on health systems strengthening have received dedicated funding announcements; and plans to restore funding to women and girls’ projects to pre-cut levels, as announced by the former International Development Secretary Liz Truss in December 2021,47 appear to have been dropped. In fact, almost a year later, in the Autumn Statement, the UK Chancellor of the Exchequer confirmed that due to continuing pressures on the budget, spending on ODA would not be restored to 0.7% until after 2027-28 at the earliest.48 At the same time, domestic expenditure of ODA on refugee costs has risen, accounting for almost a third of spending in 2022,49 further undermining the UK Government’s ability to support the SRHR of people living in the world’s poorest countries.
Around the world, the rights of women and girls are facing attacks by growing, well-funded and sophisticated anti-rights and anti-gender opposition. It is within this context that, in March 2023, the FCDO published its long-awaited update to DFID’s Strategic Vision for Gender Equality (SVGE). Addressing the global rollback on the rights of women and girls, the Women and Girls Strategy commits to taking action on ‘3 Es’: education, ending violence, and empowering women and girls and championing their health and rights, with a commitment to supporting SRHR included as part of efforts towards the latter.50 The Strategy promises to take a life-course approach, prioritising ‘neglected interventions’ including safe abortion, comprehensive sexuality education, and support for disabled women and SRHR in humanitarian emergencies.
‘It has always been abundantly clear to me that you cannot understand development if you don’t see it through the eyes of girls and women, and you cannot achieve development unless you unleash their full potential.’
- The Rt. Hon Andrew Mitchell, Minister for Development (2023)
Despite this welcome commitment and positive language on bodily autonomy in the Development Minister’s foreword, the importance of SRHR within the Strategy is undermined by the decision to include it alongside the not-insignificant projects of women’s economic and political empowerment, with minimal joined-up thinking across these objectives. Supporting women and girls to access their reproductive health and rights underpins the success of all three of the Strategy’s ambitions, and should not be confined to a single pillar. Girls with access to education, safe and sensitive contraceptive and abortion services are less likely to drop out of school. Enabling women and girls to choose whether and when they have children frees them to pursue employment and to participate more fully in social and political life. Empowering women to make decisions about their SRHR is also essential to tackling gender-based violence.
Crucially, while the Strategy recognises the need to support universal and comprehensive SRHR as a ‘long-term’ development objective, it remains unclear how this will be achieved without dedicated investment in SRHR to match. Alongside the launch of the Strategy, the UK Government announced £200 million for a new phase of its SRHR WISH programme.52 Although welcome, this represents a much smaller investment and over a longer period of time than the current WISH programme, which has in the meantime faced a further 50% cut to funding for its final year.53 There has also been a partial restoration of funding to UNFPA Supplies, with a payment of £60 million for the 2022-23 financial year.54 However, this payment does little to address the disruption to long-term projects that has already resulted from inconsistent funding. Despite its positive intentions, the UK Government ultimately remains off track to meet its 2019 commitment of £425 million, with support for UNFPA’s core operating fund remaining significantly reduced.55
5. Getting back on track
As this chapter has made clear, the UK has for some time been a significant and progressive force in support of global SRHR. While it has remained consistent in its political and diplomatic efforts, there is a disconnect between the UK’s advocacy for SRHR and the level of financial support it is currently providing.
Making donations towards SRHR in humanitarian crises is not enough. UK support must be in the form of a sustained programme that delivers against its commitments to the UN SDGs, promotes the health of women and girls as the backbone of international development, and restores the UK’s reputation as a leading global donor.
Prior to the COVID-19 pandemic, UK spending on SRHR programmes constituted 4% of the annual ODA budget, around £500 million.56 Restoring this spending every year for the next three years would make a huge contribution to supporting the 257 million women and girls who want to avoid pregnancy but who are not currently using safe, modern methods of contraception, and help to end the 121 million unintended pregnancies a year.57 Multi-year commitments such as this are essential to ensuring that progress in access to SRHR and universal health coverage can be sustained and will weather unprecedented global events. We strongly urge the UK Government to make this commitment to get back on track in its efforts to protect and promote the health of women and girls around the world.
We also recommend that the UK renew its commitment to SRHR through the FP2030 initiative. The UK’s commitment to FP2020 had a significant and meaningful impact on the global funding landscape for SRHR, and contributed to accelerating progress on addressing the unmet contraceptive needs of women and girls globally. By making a financial commitment to the FP2030 initiative, the UK Government can re-establish its leadership role on SRHR and ensure a level of accountability by linking its national actions to global-level goals and commitments.

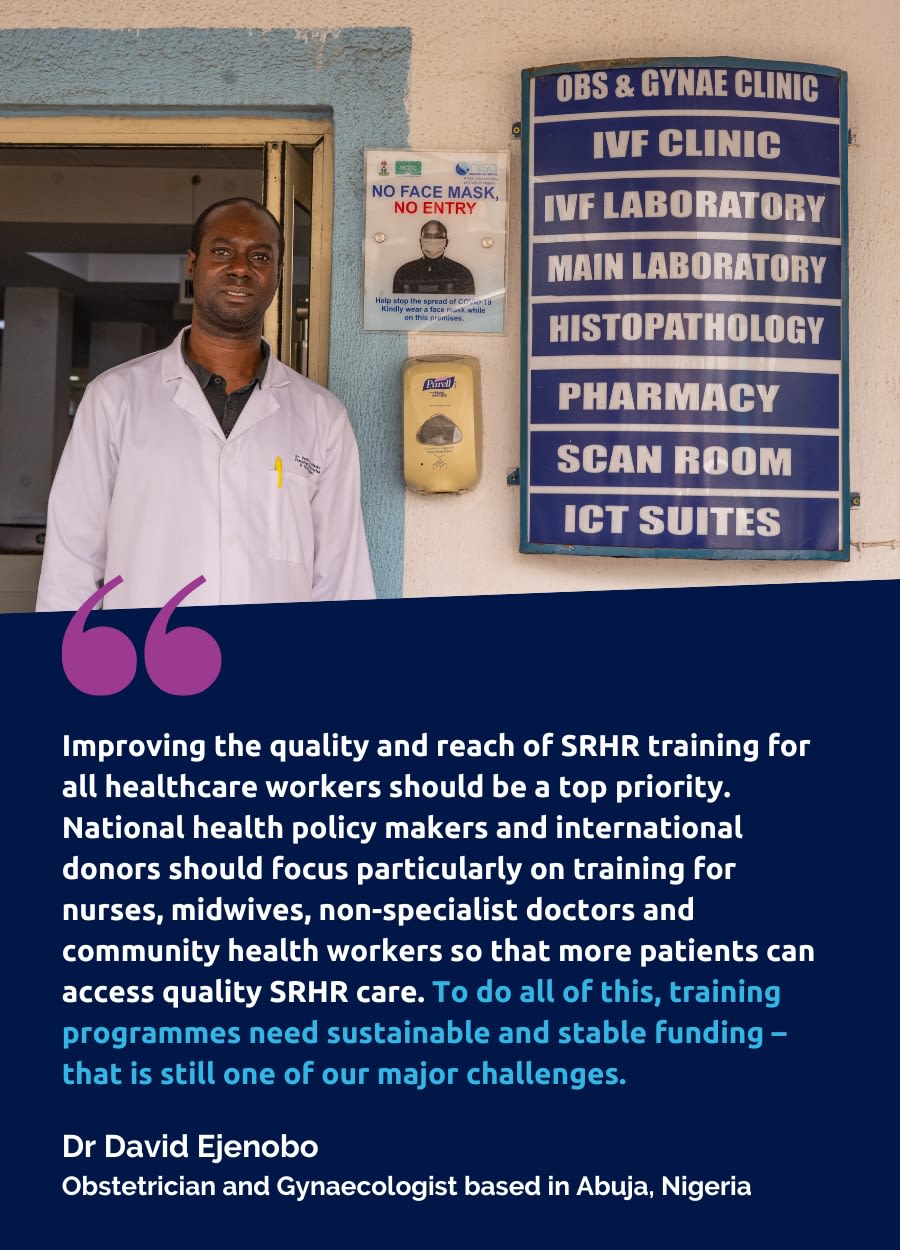
Sexual and reproductive health facility in Abuja, Nigeria
Sexual and reproductive health facility in Abuja, Nigeria

Introduction
There is a significant unmet need for SRHR services, especially in LMICs, but the investments needed to achieve universal sexual and reproductive health provision are modest and affordable.58
As part of its commitment to the SDGs, human rights and universal health coverage, the UK Government, alongside other key donors, must prioritise sufficient and long-term investment in SRHR interventions that work.59 These proven interventions expand access to quality SRHR care – with profound and lasting benefits for health outcomes and human rights. This part of the paper gives an overview of the scale of the global burden of disease, and outlines a number of impactful, innovative and cost-effective service delivery models in SRHR healthcare in low-resource settings. By targeting investment in these interventions across the life course, the UK Government and other major donors can successfully expand access to quality SRHR services for women and girls around the world.

The Partnership for Maternal, Newborn and Child Health (PMNCH), 202360
The Partnership for Maternal, Newborn and Child Health (PMNCH), 202360
1. The scale of the global burden of disease and unmet need
Encouraging progress has been made in sexual and reproductive health outcomes in recent years. This is particularly thanks to the investment behind the SDG initiative, which recognises the place of SRHR in health, gender equality and human rights.
These international efforts have led to substantial advances, including:
- From 2000-2020, the global maternal mortality rate reduced by one-third.61
- From 2015-2019, there were 121 million unintended pregnancies annually, corresponding to a global rate of 64 per 1,000 women aged 15-49. This is a decline from 79 per 1,000 women each year between 1990-1994.62
- New HIV infections have been reduced by 54% since the peak in 1996.63
Despite these gains, worldwide progress has stagnated and the uneven spread of improvements has reflected global health inequalities. A UN report from 2022 stated that ‘the world is not on track to achieve gender equality by 2030’;64 the stark global inequalities in access to quality SRHR services, the economic impact of the COVID-19 pandemic, and the global attacks on reproductive rights are all important factors in this.65 Worldwide, SRH infections and diseases are a leading cause of mortality and morbidity for women and girls,66 and there remains a staggering unmet need for SRHR services.
- Each year, over 350 million people globally need treatment for one of four curable sexually transmitted infections (STI): chlamydia, gonorrhoea, syphilis and trichomoniasis.67
- While an improvement on earlier years, the 121 million unintended pregnancies each year between 2015 and 2019 highlights the significant unmet need for contraception supplies and counselling.68
- In 2021, approximately 38 million people were living with HIV, of whom approximately 5.9 million did not know their status, UNAIDS has calculated.69
According to World Health Organization (WHO) guidelines, complications with both medical and surgical abortions are rare, as long as they are carried out safely.70 However, globally, 45% of all abortions are unsafe,71 ‘carried out either by a person lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both’.72
Targeted and sustained investment is needed to redress the pronounced global disparities in the provision of quality SRHR care, as people in LMICs bear a disproportionate burden of the unmet need. For instance, 97% of unsafe abortions take place in LMICs.73 Major disparities in contraceptive use still exist between regions, with more than half of the women and girls with unmet need for contraception living in sub-Saharan Africa and South Asia.74 The global prevalence of obstetric fistula – a preventable and treatable condition caused by prolonged and obstructed labour, which can cause incontinence, infection and psychosocial problems – is an even more striking case in point. Obstetric fistula has been almost entirely eradicated in high-income settings,75 but the WHO estimates that more than two million women and girls in countries across sub-Saharan Africa, Asia and the Pacific are living with the condition.76
As well the unmet needs outlined above, donors should prioritise the SRHR issues that have been chronically overlooked, such as menstrual and urogynaecological conditions, fibroids, endometriosis and the menopause. In research, policy, health programming and even at the point of healthcare provision, these conditions are consistently underestimated, underfunded and under-prioritised. This is despite the life-changing and often life-limiting toll they can take on those affected. There is a growing understanding of the complex interplay between reproductive health events across the life course and the risk of developing chronic disease.77 The literature also demonstrates the detrimental social and economic impact of gynaecological conditions. Research soon to be published by the RCOG shows that across LMICs, 5.35% of all years lived with disability are due to so-called ‘benign’ gynaecological conditions,78 with 84% of the overall global burden of morbidity due to these conditions found in LMICs.79
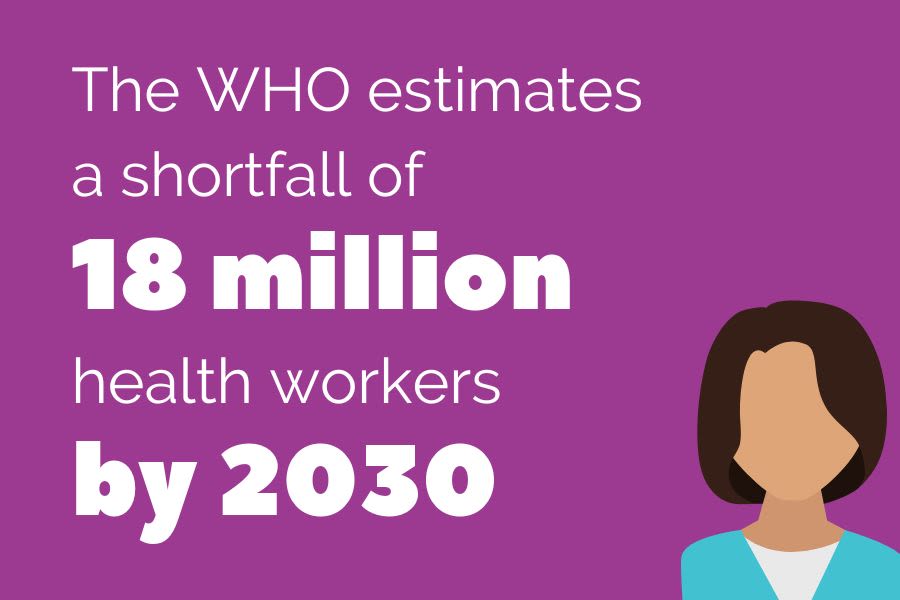
A lack of skilled workforce is a cross-cutting issue affecting SRHR service provision throughout the life course and is a major barrier to making universal health coverage a reality. The WHO estimates a shortfall of 18 million health workers by 2030, mainly in LMICs that already have the greatest shortage of trained healthcare providers and the highest maternal mortality and morbidity rates.80 A lack of skilled workforce can be a result of inadequate training for the existing workforce (in terms of quality or quantity), a lack of accessible pathways into healthcare careers for potential new recruits, and difficulties retaining well-trained workers. This multi-layered understanding of the issue makes a strong case for investment in comprehensive SRHR education across different groups and levels of healthcare workers. This would mean investing in education with adequate, evidence-based training materials, and combatting the stigma that affects health staff working in SRHR. Acknowledging the difficulties in retaining well-trained workers in LMICs also raises the question of the ethics of recruiting international healthcare workers to countries in the Global North, including the UK.
Looking deeper into global health disparities, donor-funded programmes must also address the profound inequalities in access to quality SRHR services at a local level. State provision of health coverage, to the extent that it exists in each national context, rarely includes the full range of SRHR services. Safe abortion and post-abortion care, comprehensive sexuality education, prevention and treatment of gender-based violence, and contraception and fertility care are among the services most often excluded from publicly funded schemes.81 This means that a large proportion of costs for SRHR services are paid out-of-pocket, with subsidised or free services relying on donor funding, which can often be insufficient or unreliable.82 Many people fall through the cracks: recent research has found that almost 4.3 billion people of reproductive age do not have access to even one essential reproductive health intervention over the course of their lives.83
The greatest burden of unmet need falls on marginalised groups: adolescents and children, rural communities, sex workers, LGBTQ+ people, older people, racialised minorities and disabled people, among others, are consistently underserved by SRHR services across diverse national contexts. For instance, adolescents in LMICs have a disproportionate unmet need for contraception counselling and supplies; together with a lack of comprehensive sex and relationships education, and other logistical and social barriers to SRHR care, this means that the level of unplanned pregnancy and STIs among young people continues to be a major concern.84 By providing SRHR services with the trained staff and resources required, key donors like the UK Government can take vital strides towards meeting the needs of these typically underserved groups.
2. The case for investment in SRHR: investing in service delivery models that work
To address current levels of unmet need for quality SRHR services around the world, the UK Government and other donors need to commit to scaling up targeted investment in evidence-based service delivery models.
This investment should embrace the Guttmacher-Lancet Commission definition of SRHR as an integral and interdependent range of health issues. Within this framework, SRHR funding should be channelled towards prevention and early treatment interventions, strengthening the health workforce and expanding access to quality SRHR services for women and girls at every stage of life.
The Guttmacher-Lancet Commission definition of SRHR: ‘Sexual and reproductive health is a state of physical, emotional, mental, and social wellbeing in relation to all aspects of sexuality and reproduction, not merely the absence of disease, dysfunction, or infirmity. Therefore, a positive approach to sexuality and reproduction should recognise the part played by pleasurable sexual relationships, trust, and communication in the promotion of self-esteem and overall wellbeing. All individuals have a right to make decisions governing their bodies and to access services that support that right.’
Source: Starrs A.M. et al. (2018). Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. The Lancet, Vol. 391, Issue 10140, 2642–2692. https://doi.org/10.1016/S0140-6736(18)30293-9
2.1 Counselling and services for contraception
In 2022, more than 164 million women and adolescents had unmet need for contraception, despite significant progress and global investment in the use of modern contraceptives worldwide over the previous 50 years.85

Sexual and reproductive health facility in Abuja, Nigeria
Sexual and reproductive health facility in Abuja, Nigeria.
Increased investment in task sharing and task shifting for healthcare professionals and integrated service delivery is needed to urgently expand access to contraceptive services. The UK Government has an excellent track record of expanding access to contraceptives, including through its flagship Reproductive Health Supplies and WISH programmes. The UK Government should build on this important work with additional targeted investment in the interventions outlined below.
Expanding access through task sharing and task shifting
Contraception is an inexpensive and cost-effective intervention that enables women and girls to exercise their bodily autonomy and reproductive rights. However, health workforce shortages and restrictive policies on the roles of mid- and lower-level professionals limit access to effective contraceptive methods in many settings. Task shifting and task sharing are effective solutions to this problem that the UK Government and other donors should prioritise for investment.
Task shifting/sharing is defined by the WHO as the redistribution of specific tasks among healthcare teams, from highly qualified health workers to health workers with shorter training and fewer qualifications, in order to make more efficient use of the available human resources for health, thereby increasing access to quality healthcare.86
Task sharing is a tried and tested strategy87 that addresses the shortage and maldistribution of health workers to help achieve more equal access to contraception services, particularly for typically underserved groups such as young and poor women, LGBTQ+ people, unmarried women, older women, migrants, and those living in rural areas.88, 89 Crucially, by expanding the reach of contraception services, task shifting can provide women and girls with more options around methods; as long as services are well resourced, health workers can counsel service users and help them decide upon their preferred method of contraception.90 Access to a diverse range of contraception supplies and the necessary information to make a choice about their preferred method is vital for women and girls’ bodily autonomy and contraception efficacy.91
Strengthening integrated service delivery
Integrating contraception services into wider healthcare services is an important and cost-effective way of reaching those who would otherwise have an unmet need for contraception.92 It should be at the core of the UK and other donor governments’ investments.
Women and girls in LMICs seeking to postpone or space pregnancy have a particularly high unmet need for contraception. Integrating services involves offering voluntary contraception counselling at key ‘touch points’ when patients come into contact with health workers for other services such as perinatal care, post-abortion care and childhood immunisation. Offering modern contraception services as part of perinatal care and early childhood immunisation increases postpartum contraceptive use; it is likely to reduce both unintended pregnancies and pregnancies that are too closely spaced, which have detrimental effects on maternal and neonatal health outcomes.
Scaling up access to contraceptives through task sharing in Africa: A 2021 study conducted in conjunction with the WHO across Burkina Faso, Cote d’Ivoire, Ethiopia, Ghana and Nigeria identified a number of task sharing interventions that supported an increase in contraceptive uptake and access to contraception counselling services. In Burkina Faso, the Ministry of Health provided community health workers (CHWs) and midwives with comprehensive specific training needed for performing new family planning tasks. As a result, uptake of LARC increased by more than three times within a period of six months, with 232.9% new implant users and 163.0% new intrauterine contraceptive device (IUCD) users. There were also marked improvements in access to contraceptive injections and contraceptive pills: a 40.1% and 23.7% increase in users, respectively. Most importantly, the new contraception programme averted 11.7% of projected unintended pregnancies in 2019. For a more sustainable impact, the programme set up mechanisms for post-training follow-up, monitoring and evaluation, and quality control. To complement workforce strengthening, it also included advocacy meetings and community mass mobilisation campaigns.
Source: Ouedraogo L. et al. (2021). Towards achieving the family planning targets in the African region: a rapid review of task sharing policies. Reprod Health 18, 22. https://doi.org/10.1186/s12978-020-01038-y
2.2 Safe abortion services and post-abortion care
Thanks to key donors like the UK Government, recent years have seen significant advancements in access to safe abortion. Well-resourced SRHR programmes that integrate abortion care have been a driving force of this progress.
For instance, the UK Government’s multi-country WISH programme has helped to avert 4.3 million unsafe abortions and over 22,000 maternal deaths.93
Yet many people still have an unmet need for safe and quality abortion care.94 Greater investment is needed in interventions that increase access to quality comprehensive abortion care within an enabling environment. The ‘enabling environment’ for quality abortion care is founded on respect for human rights, including a supportive framework of law and policy, the availability and accessibility of information, and a universally accessible, affordable and well-functioning health system.95
Expanding access to safe abortion through nurses and midwives in Nepal: A pilot programme in Nepal supported 20 government health posts to expand access to safe abortion to underserved communities in 20 rural municipalities, by training auxiliary nurses and midwives (ANMs) in the provision of medical abortion. The programme provided more services in the first six months of 2016 (353) than in the whole of 2015 (340), addressing the considerable unmet need for quality abortion care. The first key element that made the programme successful was a comprehensive regulatory framework that defined the legislation, clinical norms and regulations. The second was the inclusion of mid-level providers in the provision of safe abortion services: the programme worked with a National Health Training Centre that trained ANMs and community health workers on medical abortion provision. This training brought abortion care expertise into primary health facilities and in-community care, which in turn increased awareness among communities on the availability of medical abortion services and access to quality care. The programme also supported provider buy-in by giving adequate remuneration for the increase in workload, and ensured regular and reliable delivery of medical abortion drugs.
Source: Safe Abortion Action Fund (2017). Using the task sharing model to expand access to safe abortion services to under-served populations in Nepal. https://www.safeaccesshub.org/media/1025/saaf_nepal_web.pdf?mode=pad&rnd=131994531020000000
Including abortion in mainstream healthcare
Expanding abortion care provision to a wider range of providers and health facilities to reduce current rates of unsafe abortion needs far greater investment. In many national contexts, however, it also requires changes to abortion laws, policies and guidelines to remove restrictive and unnecessary legal, clinical and policy barriers and to adequately invest in health worker training, especially where abortion has been excluded from the foundational medical and health professional training curricula. Greater investment in integrating abortion services within mainstream maternity and women’s health services is a key intervention to help expand access to quality abortion care, and minimises the stigma associated with abortion care for both patients and providers. This mainstreaming approach, which treats abortion purely as a form of healthcare, must be at the heart of all UK Government funded SRHR programmes.
Investing in telemedicine for abortion care
Telemedicine is the remote assessment and treatment of patients by means of telecommunications technology. It is increasingly being used as an effective service delivery model that warrants greater attention and investment across different areas of SRHR and beyond,96 particularly in the wake of COVID-19 lockdowns. WHO guidance states that people can safely self-manage medical abortion as long as they have accurate information and access to health services, should they need or want them during the abortion service.97 Telemedicine is an effective way for health professionals to provide that information, and an important emerging area for greater investment from the UK Government and other donors.
South Africa’s telemedicine success story: Recent studies on South Africa’s expansion of telemedicine abortion services have found it to be a highly effective and safe service delivery model and that telemedicine has increased privacy, reduced the experience of stigma and enabled a relationship with a trusted online provider. The service delivery models in both of the South African programmes studied combine telemedicine with some in-person care. This goes to show that the terms ‘telemedicine’ and ‘self-management’ include a whole spectrum of service delivery models. Within these categories, there are a range of options to fit different legal requirements, the availability of trained health workers, and the specific barriers facing those who are trying to access abortion care in a given setting.
Sources: Margit Endler et al. (2022). A telemedicine model for abortion in South Africa: a randomised, controlled, non-inferiority trial, The Lancet, Vol. 400, Issue 10353, 670-679. https://doi.org/10.1016/S0140-6736(22)01474-X; and Oluwaseyi Dolapo Somefun et al. (2023). The acceptability of implementing telemedicine for early medical abortion in South Africa: A substudy to a randomized controlled trial. SSM - Qualitative Research in Health, Vol. 3, 100241. https://doi.org/10.1016/j.ssmqr.2023.100241
2.3 Gynaecological health conditions
The UK and other donors must work to redress the consistent deprioritisation of so-called ‘benign’ gynaecological conditions.
Long-term underfunding has left millions of women and girls around the world suffering with life-changing and often life-limiting conditions, and led to a staggering unmet need for quality gynaecological healthcare. The term ‘benign gynaecological conditions’ refers to uterine fibroids, polycystic ovary syndrome, female infertility, genital prolapse, endometriosis, miscarriage and abortion, ectopic pregnancy, pelvic inflammatory disease and ‘other gynaecological diseases’, such as menstrual conditions and non-menstrual conditions including inflammatory diseases of the cervix.
Equipping health workers to address gynaecological disease
Preventive and curative services for gynaecological diseases, and particularly menstrual conditions, are still not explicitly addressed in national health policy and training curricula, and they are consistently overlooked in donor-funded programmes.98 In many places, this means that women and girls experience long delays and barriers to diagnosis. Even after diagnosis, many are unable to access quality clinical care when they experience gynaecological health problems. So investing in health worker training on gynaecological health must be a top priority for the UK and other donors. Training that equips health workers to recognise, prevent and treat gynaecological disease at the earlier stage is a cost-effective and important approach to addressing the global burden of gynaecological disease.
Taking a cross-cadre approach to tackling gynaecological disease: The RCOG’s Gynaecological Health Matters (GHM) programme delivers a cost-effective and targeted approach to up-skilling healthcare professionals, equipping non-specialist SRH service providers such as nurses and non-specialised doctors with the skills necessary to recognise and treat a range of gynaecological conditions. This ‘cross-cadre’ approach ensures that patients can access quality gynaecological healthcare at the primary care level and from community health workers. The training consists of 11 modules that focus on topics that are often lower priorities in national training curricula but that represent a significant burden of disease and unmet need. These include cervical cancer, contraception, infertility, early pregnancy loss, obstetric fistula and gender-based violence.
In Bangladesh, the GHM programme has partnered with icddrb and the Obstetrical and Gynaecological Society of Bangladesh (OGSB) to train nurses and newly recruited non-specialist doctors in the districts of Kushtia and Dinajpur. To foster long-term, sustainable advances in gynaecological health, the programme is also working with a group of ‘Champions’ to advocate for the adoption and roll-out of the training package across the country’s health system and the founding of a national registry to monitor the prevalence of gynaecological conditions and health outcomes for those affected. In the words of Dr Ashutosh Deb Sharma, a Senior Consultant and GHM trainer in Dinajpur, ‘We are facing a lack of resources and a limited number of trained healthcare professionals: these are the main barriers to quality healthcare facing women and girls in my district… Programmes like the Essential Gynaecological Skills training provide us with so much. It fills the gaps in our knowledge and skills. This will help us to provide better gynaecological health services to women and girls at the primary care level.’
Source: RCOG. Our Gynaecological Health Matters Programme. https://www.rcog.org.uk/about-us/global-network/centre-for-womens-global-health/gynaecological-health/our-gynaecological-health-matters-programme/
2.4 Prevention, detection and management of gynaecological and reproductive cancers
Cervical cancer is a largely preventable and curable disease. Interventions including human papillomavirus (HPV) vaccination, cervical screening, and early diagnosis and treatment of cancer are effective99 and low-cost.100
However, in many low-resource settings access to effective cervical cancer prevention and treatment strategies remains extremely limited.101, 102 Regarding other gynaecological cancers, currently there are no reliable or effective screening tests for ovarian, vulvar, uterine or vaginal cancers, resulting in late presentation and diagnosis. A lack of public awareness and understanding of these cancers, and a lack of accessible and effective treatment options, are responsible for the higher mortality rate. Greater investment in approaches such as HPV vaccination and a screen-and-treat system can significantly reduce the numbers of women dying from gynaecological and reproductive cancers in LMICs.
Prevention first: expanding access to HPV vaccination
In 2020, the WHO launched a Global Strategy to Accelerate the Elimination of Cervical Cancer. This outlines three key steps:103

This three-point plan clearly stresses the importance of a prevention-first approach. To back this global initiative, key donors like the UK Government must invest in HPV vaccination as an immediate priority. Increasing coverage of HPV vaccination in LMICs requires sufficient and affordable supply of HPV vaccines to meet population needs at a country level. Efficient and sustainable multisectoral delivery models work best and should be the focus of greater investment: these include school immunisation programmes, innovative community-based approaches to reach underserved populations (such as adolescent girls who are not in school), and evidence-based communication and social mobilisation efforts to address barriers to the acceptance and uptake of the vaccine.104, 105
A comprehensive approach to HPV vaccination in Rwanda: Rwanda’s national HPV vaccination programme is an exemplar of the comprehensive approach required for success: multiple streams have been built into the programme to reach the highest number of girls and young women for HPV vaccination. In 2011, Rwanda integrated HPV vaccinations for all girls in grade six of primary school, for free, on three designated ‘health days’ each year. HPV vaccines were provided during health days for deworming all children in primary schools and during Rwanda’s annual Maternal and Child Health Week. These health days were also used to disseminate essential messages on adolescent health to this underserved age group. In parallel, teachers and community leaders were included in sensitisation sessions, and the country’s 45,000 community health workers were mobilised to trace out-of-school girls, who are often missed by adolescent health initiatives. This multi-pronged approach meant that the HPV vaccination programme reached 92,107 (93.2%) of the 98, 792 eligible girls identified in its first year.
Source: Sayinzoga F. et al. (2020). Human papillomavirus vaccine coverage in Rwanda: A population-level analysis by birth cohort. Vaccine. 38(24):4001-4005. https://doi.org/10.1016/j.vaccine.2020.04.021
Investing in a screen-and-treat approach
A number of sub-Saharan African countries promote a single-visit screen-and-treat approach for cervical screening and preventive treatment. This innovative approach is highly effective, as it mitigates the high cost and inconvenience that patients often incur with referrals to tertiary care facilities and reduces the risk of patients dropping out between appointments.
A recent pilot programme in Cameroon is a compelling example of how cervical cancer prevention, screening and treatment can be combined. The programme incorporated the principles of self-sampling, screen-and-treat integration and task sharing106 to dramatically increase compliance with a screening programme in a low-resource setting. The pilot demonstrated that self-sampling improves patients’ experience of cervical cancer treatment by affirming their bodily autonomy and participation in their own healthcare.107
As the Cameroon example demonstrates, single-visit screen-and-treat models make the case for task sharing and task shifting within cervical cancer service delivery, as this approach includes nurses and community health workers who are trained to expand access to remote areas without tertiary care facilities. The impact of this approach has also been seen at the Dhaka Medical College Hospital, a 2,600-bed government hospital in Bangladesh:

With stable and sufficient support from donors, task shifting to community health workers has the potential to increase screening coverage and treatment uptake in resource-limited settings and is an important area for investment.
2.5 Prevention and treatment of HIV and other sexually transmitted infections
In 2020, the WHO estimated 374 million new infections with one of four STIs: chlamydia (129 million), gonorrhoea (82 million), syphilis (7.1 million) and trichomoniasis (156 million).
Left untreated, these STIs can have adverse effects on sexual and reproductive health, including infertility, chronic pelvic pain and psychosexual problems, as well as posing a substantial economic burden. STI care still does not reach the most vulnerable people, especially in LMICs with high HIV burden. The expansion of antiretroviral therapy has made important advances in recent years, leading to a 48% decline in deaths from AIDS-related causes. But AIDS-related illnesses still remain a leading cause of death among women of reproductive age (15-49 years), particularly in sub-Saharan Africa.108 Due to social stigma and pervasive misconceptions about age and sexual activity, both adolescents and older women are typically overlooked in STI education, prevention and detection programmes.109, 110
Point-of-care testing (POCT) and integrated HIV services are two key interventions that address the unmet need for prevention, detection and treatment of STIs and HIV. These interventions put the interlinked understanding of SRHR into action and are highly effective. They need continued investment from donors, including the UK Government, as part of comprehensive SRHR programmes.
Building capacity for point-of-care testing
POCT around pregnancy can support more effective management of STIs. Routine screening during the pre-natal and post-natal period is an effective intervention that supports prevention of vertical (parent to baby) transmission and helps mitigate the parent’s risks associated with pregnancy and birth.
A recent systematic review of POCT in low-resource settings showed that integrating syphilis testing into perinatal care garnered significantly higher testing and treatment rates as well as a marked improvement in pregnancy outcomes, compared to laboratory screening.111 Availability of an adequate and trained health workforce is the key to realising the potential of POCT; long-term investment in health worker training must, therefore, be a priority for the UK Government and other donors looking to address unmet need for STI care. Furthermore, unreliable supply chains pose a significant problem for the provision of POCT. Robust funding, procurement and supply chain processes are essential to ensure an uninterrupted supply of consumables for both testing and treatment, so that populations receive appropriate care.112
Strengthening integrated HIV services
More than one million HIV-positive women of reproductive age become pregnant globally each year.113 Recent years have seen encouraging advances in antiretroviral therapy (ART). However, keeping HIV-positive women retained in care, adherent to ART and with HIV viral suppression is a major public health challenge, particularly postpartum. One effective solution is the integration of ART into obstetric and postpartum care, including training health workers in these services on the barriers to ART adherence during the postpartum period.
Integrating antiretroviral therapy into maternity care in South Africa: A randomised control trial in South Africa compared an integrated post-natal service among mothers and their infants to the local standard of care. The former included immediate post-natal referral of HIV positive women on ART to general adult ART services, and their infants to separate routine infant follow-up. The study showed that 77% of women in the integrated intervention were ART adherent and had viral suppression at 12 months postpartum, compared to 56% of women receiving standard care. The lessons from this study can also be applied to care for menopausal women living with HIV. As ART has become more effective and more widely available, HIV has been transformed from a life-limiting condition into one with near-normal life expectancy. As the population of older women living with HIV continues to increase, it is important that HIV management adapts to the unique challenges that women with HIV face with regards to engagement with HIV care across the life course. A holistic clinical approach that addresses the multidimensional nature of menopausal symptoms may support midlife women living with HIV in maintaining optimal adherence to ART and clinic attendance.
Sources: Myer L. et al. (2018). Integration of postpartum healthcare services for HIV-infected women and their infants in South Africa: a randomised controlled trial. PLoS medicine. 30;15(3):e1002547; and Solomon D. et al. (2021). The association between severe menopausal symptoms and engagement with HIV care and treatment in women living with HIV. AIDS Care, 33:1, 101-108, https://doi.org/10.1080/09540121.2020.1748559
2.6 Female genital mutilation
FGM is a human rights violation and a severe form of violence against women and girls.
FGM is inflicted mainly on young girls sometime between infancy and adolescence. More than 200 million girls and women alive today have gone through some form of FGM, and a further 68 million are at risk of being cut by 2030.114 These women mostly live in 30 countries in Africa, the Middle East and Asia where this practice is concentrated. In some of these countries, such as in Egypt, FGM is increasingly being carried out by doctors. The UK Government has made important contributions in challenging gender-based violence and FGM around the world, including through its support to the Africa-led Movement to End FGM. With rates of medicalised FGM rising, it can play an even stronger role working with healthcare professionals to end this practice.
Supporting health workers in their efforts to eradicate FGM
As influential figures in their communities, doctors and healthcare workers have a key role to play in eradicating FGM and promoting the sexual and reproductive rights of women and girls. For that reason, and in light of the increasing medicalisation of the practice, FGM-prevention programmes should engage the medical community as key stakeholders. Working with health professions would be an impactful complement to the UK Government’s existing approaches to ending FGM, which focus predominantly on shifting social norms in affected communities. Training programmes that equip health workers with the skills, competencies and attitudes to advocate against FGM in their communities are a key prevention strategy that merit long-term investment. The UK Government and other investors in SRHR should seek to collaborate with medical bodies and colleges, such as the RCOG, who can mobilise large global networks of healthcare professionals to tackle the rising medicalisation of FGM.
2.7 Urogynaecology, including fistula
Obstetric fistula is a neglected public health and human rights issue.
There is a stark global inequality in the burden of obstetric fistula: this preventable and treatable condition has been almost entirely eradicated in high-income settings, but it is estimated that around two million women and girls in 60 LMICs currently live with a fistula, and that 50,000-100,000 new cases develop each year. Obstetric fistula is caused by unrelieved obstructed labour, which results in a hole between the vagina and the bladder and/or rectum. The condition leads to chronic incontinence and has a severe psychosocial impact. There is a vital need for comprehensive investment in prevention, emergency obstetric skills and referral pathways, and fistula repair training.115

Investing in the prevention of obstetric fistula
The UK and other donors need to invest in interventions that prevent obstetric fistula. This means long-term and well-funded programmes to train healthcare workers in emergency obstetric skills and to strengthen referral pathways for cases of prolonged and obstructed labour.116 To complement that health system strengthening, obstetric fistula programmes should incorporate even earlier interventions to mitigate a key risk factor for obstetric fistula: childbearing at a young age.117 Access to contraception services, including counselling and a range of supplies, is an important fistula prevention strategy.118 Obstetric fistula programmes should invest in contraception services that reach out to typically underserved groups including young people, out-of-school girls and those living in rural communities. Likewise, contraception services should include information about obstetric fistula in their counselling.
Comprehensive sexuality education (CSE) is another vital element of obstetric fistula prevention. CSE programmes should engage young people in schools and reach out-of-school adolescents and people throughout the life course as part of public health information campaigns.119, 120 Not only is CSE an effective way of sharing information about contraceptive options; a truly comprehensive, gender-transformative CSE model121 also includes information on gender-based violence and child marriage, which are risk factors for obstetric fistula. This model combining adolescent inclusion and early intervention fulfils women and girls’ reproductive and sexual rights, mitigates the risk of obstructed and prolonged labour, and delivers a more cost-effective approach to obstetric fistula prevention.
Equipping medical specialists with skills to repair obstetric fistula: The International Federation of Gynecology and Obstetrics (FIGO) Fistula Training Initiative is working to scale up global treatment efforts by helping to train more fistula surgeons (and holistic care teams). It supports increasing fistula treatment capacity globally and in-country by training eligible medical specialists (obstetric gynaecologists, general surgeons and urology specialists) as well as training a group of Fellows to trainer level. The programme has a success rate of 84% for obstetric fistula closure and is implemented in 26 countries across sub-Saharan Africa and Asia. Key learnings from the programme that support sustainable and effective obstetric fistula management include: ensuring that the training is flexible, allowing Fellows to accommodate their professional responsibilities unrelated to obstetric fistula repair, which supports retention on the course; providing tailored coaching visits to support trainee Fellows to refine their skills; and strengthening the fistula treatment chain.
Source: FIGO. Fistula Surgery Training Initiative. https://www.figo.org/what-we-do/obstetric-fistula/fistula-surgery-training-initiative; and Slinger G. and Trautvetter L. (2020). Addressing the fistula treatment gap and rising to the 2030 challenge. Int J Gynecol Obstet, 148: 9-15. https://doi.org/10.1002/ijgo.13033
Strengthening fistula surgery training
The global effort to eradicate obstetric fistula needs to move away from short-term interventions and towards a sustainable and comprehensive package of prevention, treatment and follow-up care.122 Obstetric and vesico vaginal fistulas can be repaired, but due to a global shortage of fistula surgeons only one woman in 50 receives a fistula repair.123 There are two key factors impeding fistula treatment: the absence of both a widely agreed curriculum and a co-ordinated international training programme for fistula surgeons. To address these barriers, donors need to work with international standard-setting bodies and national health worker professional bodies to embed high-quality, evidence-based fistula training into national curricula.124, 125 To improve access to quality fistula care in the long term, these programmes need sustained investment.


Recommendations
As the 2030 deadline for achieving the UN SDGs approaches, the UK Government has a critical role to play in promoting global SRHR.
Alongside continuing to advocate for the rights of women and girls, the UK Government must prioritise sufficient and long-term investment in effective SRHR interventions to deliver its agenda for gender equality as set out in the Women and Girls Strategy. By taking a comprehensive approach that recognises the SRHR of women and girls throughout the life course, the UK Government can ensure that its investment will have the greatest impact and will successfully expand access to quality SRHR services for women and girls around the world.
The Royal College of Obstetricians and Gynaecologists is calling on the UK Government to:
1. Make the commitments of the Women and Girls Strategy a reality by increasing investment in SRHR:
- Restore ODA to 0.7% of GNI in 2024-25 and commit to 0.7% for the next 10 years.
- Ring-fence the equivalent of 0.5% GNI for expenditure on development assistance delivered outside the UK.
- Spend £500 million per year for the next three years in SRHR programming and supplies.
- Publish clear spending targets and timelines for SRHR and gender equality, including how it will deliver on its 2021 commitment to restoring funding for women and girls.
2. Strengthen the UK’s global advocacy on SRHR by investing in new and existing global partnerships and collaborations, particularly on stigmatised issues:
- Restore support to the UNFPA core operating fund alongside existing commitments to its Supplies Partnership, to ensure future stability in global SRHR supply chains.
- Renew the UK’s commitment to the FP2030 initiative.
- Champion the integration of abortion care into sexual and reproductive health services through the FCDO’s programmes and through national universal healthcare plans as part of health system strengthening efforts.
- Champion prioritisation of the gynaecological health needs of women and girls on the global health agenda, to influence the investment of other donors.
- Build on commitments to tackling FGM by collaborating with medical bodies and colleges to create a global network of health workers to tackle rising medicalisation.
3. Ensure that the life-course approach of the Women and Girls Strategy is truly comprehensive by targeting investment in evidence-based, scalable interventions:
- Scale up self-management and telemedicine in settings where it can provide safe additional pathways to increase access to SRHR.
- Collect data and research on the scale of the burden of gynaecological disease across the life course for women and girls, to build a strong evidence base to support future investment.
- Integrate contraception services into maternal services, post-abortion care and childhood immunisation programmes.
- Strengthen HPV immunisation programmes in LMICs.
- Develop and deliver high-quality, evidence-based fistula repair and emergency obstetric training.
4. Invest in task shifting and task sharing for health workers as part of commitments to strengthening health systems, to support the delivery of comprehensive and integrated SRHR services:
- Publish clear spending plans and timelines for health systems strengthening.
- Invest in training for non-specialist healthcare providers to diagnose, prevent and treat gynaecological disease at an early stage.
- Invest in training a wider range of providers and health facilities to support the expansion of abortion care provision.
- Invest in supporting task shifting for long-acting reversible contraception (LARC) to expand access where feasible.

References
1. GOV.UK (2022, Oct 19). We must respect the bodily autonomy of women and girls throughout their lives. Speech. Cross-regional joint statement at the UN Third Committee. https://www.gov.uk/government/speeches/we-must-respect-the-bodily-autonomy-of-women-and-girls-throughout-their-lives-cross-regional-joint-statement-at-the-un-third-committee
2. United Nations Population Fund (2022). Investing in three transformative results: Realizing powerful returns. New York. https://www.unfpa.org/sites/default/files/pub-pdf/Realizing%20powerful%20returns_EN_FINAL.pdf
3. DSW and European Parliamentary Forum for Sexual & Reproductive Rights (n.d.). Donors Delivering for SRHR: Report 2020. Tracking OECD Donor Funding for Sexual and Reproductive Health and Rights. https://donorsdelivering.report/wp-content/uploads/2021/09/DD_Report_2020.pdf
4. GOV.UK (2012, July 11). Family planning: Historic breakthrough for 120m women. News story.https://www.gov.uk/government/news/family-planning-historic-breakthrough-for-120m-women
5. GOV.UK (2012, July 11). Family planning: UK aid saves a woman’s life every two hours. News story.https://www.gov.uk/government/news/family-planning-uk-aid-saves-a-woman-s-life-every-two-hours
6. GOV.UK (2015, Sept 25). Britain backs the Global Goals for Sustainable Development. News story. https://www.gov.uk/government/news/greening-britain-backs-the-global-goals-for-sustainable-development
7. GOV.UK (updated 2019, March 6). Leaving no one behind: Our promise. Policy paper. https://www.gov.uk/government/publications/leaving-no-one-behind-our-promise/leaving-no-one-behind-our-promise
8. Ibid.
9. FP2020 (update 2017, Sept 20). Summary of Commitments. Family Planning Summit 11 July 2017, London. https://fp2030.org/sites/default/files/FP_Summit_2017_Commitment_Summary_Update-V18-Clean_9.pdf
10. UK Aid (2017, July 11). Summary of UK Commitments. Family Planning Summit 11 July 2017, London. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/644641/Family-Planning-Summary1.pdf
11. UK Parliament. (2022, Dec 7). Development Aid: Genito-urinary Medicine and UN Population Fund. Question for Foreign, Commonwealth and Development Office. https://questions-statements.parliament.uk/written-questions/detail/2022-12-07/105263
12. GOV.UK (2017, July 11). Priti Patel: Family Planning Summit speech at the London Family Planning Summit #HerFuture. https://www.gov.uk/government/speeches/family-planning-summit
13. GOV.UK. (2018). DFID Strategic Vision for Gender Equality: Her Potential, Our Future. Policy paper. https://www.gov.uk/government/publications/dfid-strategic-vision-for-gender-equality-her-potential-our-future
14. DFID (2018). DFID Strategic Vision for Gender Equality: A Call to Action for Her Potential, Our Future. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/708116/Strategic-vision-gender-equality1.pdf
15. The Foreign Commonwealth and Development Office was created on 2 September 2020 through the merger of the Foreign and Commonwealth Office and the Department for International Development.
16. IPPF (n.d.). About WISH: Leaving no one behind. https://www.ippf.org/about-wish#
17. GOV.UK (2019, April 8). Penny Mordaunt on improving sexual health rights globally. Speech. https://www.gov.uk/government/speeches/penny-mordaunt-on-improving-sexual-health-rights-globally
18. IPPF (n.d.). Programme: Access. https://www.ippf.org/our-approach/programmes/access
19. IPPF (n.d.). UK International Development Committee inquiry: FCDO’s approach to sexual and reproductive health. https://committees.parliament.uk/writtenevidence/120306/pdf/
20. UK endorsement of Guttmacher-Lancet definition of SRHR. (2019, Nov 1). The Nairobi Summit Commitments on ICPD25. https://www.nairobisummiticpd.org/commitment/endorsement-guttmacher-lancet-definition-srhr
21. Starrs A.M. et al. (2018). Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. The Lancet, Vol. 391, Issue 10140, 2642–2692. https://www.guttmacher.org/guttmacher-lancet-commission/accelerate-progress-executive-summary
22. GOV.UK (2019, Sept 23). Healthcare for everyone must prioritise women’s sexual and reproductive health and rights, says UK at UN General Assembly. Press release. https://www.gov.uk/government/news/healthcare-for-everyone-must-prioritise-womens-sexual-and-reproductive-health-and-rights-says-uk-at-un-general-assembly
23. UNFPA (2020, Oct 14). United Kingdom commits £425 million to family planning, preventing millions of unintended pregnancies and hundreds of thousands of deaths worldwide. https://www.unfpa.org/updates/united-kingdom-commits-425-million-family-planning-preventing-millions-unintended
24. UN Women (2020, April 9). Policy Brief: The Impact of COVID-19 on Women. https://www.unwomen.org/sites/default/files/Headquarters/Attachments/Sections/Library/Publications/2020/Policy-brief-The-impact-of-COVID-19-on-women-en.pdf
25. Zulaika G., Bulbarelli M., Nyothach E. et al. (2022). Impact of COVID-19 lockdowns on adolescent pregnancy and school dropout among secondary schoolgirls in Kenya. BMJ Global Health 2022;7:e007666. https://gh.bmj.com/content/7/1/e007666
26. UN Women (2020). COVID-19 and Ending Violence Against Women and Girls. https://perma.cc/G48D-BVCU
27. UNFPA (2021, March 11). Impact of COVID-19 on Family Planning: What we know one year into the pandemic. Technical note. https://www.unfpa.org/sites/default/files/resource-pdf/COVID_Impact_FP_V5.pdf
28. MSI Reproductive Choices (2020, August 19). Press release: 1.9m clients lost access to our services due to COVID-19. https://www.msichoices.org/news-and-insights/news/2020/8/press-release-19m-clients-lost-access-to-our-services-due-to-covid-19/
29. GOV.UK (2020, Nov 26). Changes to the UK’s aid budget in the Spending Review: UK aid will be overhauled to achieve greater impact. News story. https://www.gov.uk/government/news/changes-to-the-uks-aid-budget-in-the-spending-review
30. GOV.UK (2023, March 15). National statistics. Statistics on International Development: final UK aid spend 2021. https://www.gov.uk/government/statistics/statistics-on-international-development-final-uk-aid-spend-2021/statistics-on-international-development-final-uk-aid-spend-2021#:~:text=The%20decrease%20in%202021%20ODA,spend%20in%202013%20and%202014
31. The Telegraph (2022, April 12). UK the only G7 country to cut aid during Covid pandemic: Government confirms UK’s excess Covid vaccine donations were taken from aid budget. https://www.telegraph.co.uk/global-health/climate-and-people/uk-g7-country-cut-aid-covid-pandemic/
32. THET (2021, May 20). Press Release: Government cuts £48million in funding for global health training as part of UK Aid spending cuts. https://www.thet.org/press-release-government-cuts-48million-in-funding-for-global-health-training-as-part-of-uk-aid-spending-cuts/
33. The Guardian (2023, March 16). Behind the fanfare of James Cleverly’s visit to Sierra Leone, the need to restore aid is starkly apparent. https://www.theguardian.com/global-development/2023/mar/16/behind-the-fanfare-of-james-cleverlys-visit-to-sierra-leone-the-need-to-restore-aid-is-starkly-apparent
34. UNFPA (n.d.). Donor contributions: United Kingdom of Great Britain and Northern Ireland. https://www.unfpa.org/donor/united-kingdom-great-britain-and-northern-ireland
35. Written evidence of 18 April 2023 submitted by Matt Jackson, Chief, London Representation Office. UNFPA. https://committees.parliament.uk/writtenevidence/120313/default/
36. UK Parliament (2023, April 18). Development Aid: Genito-urinary Medicine. Question for Foreign, Commonwealth and Development Office, UIN 181199. https://questions-statements.parliament.uk/written-questions/detail/2023-04-18/181199
37. Baldoumas A. (2021, May 20). UK aid cuts: little information but devastating consequences. Bond. https://www.bond.org.uk/news/2021/05/uk-aid-cuts-little-information-but-devastating-consequences/
38. Devex. (2021, Nov 19). UK assessment predicted aid cuts would hurt gender equality programs. https://www.devex.com/news/uk-assessment-predicted-aid-cuts-would-hurt-gender-equality-programs-102097
39. Guttmacher Institute (2021, Oct 21). Just the Numbers: Impact of UK Sexual and Reproductive Health Funding for Family Planning, Fiscal Year 2021–2022. https://www.guttmacher.org/just-numbers-impact-uk-international-family-planning-assistance-2021-2022
40. Written evidence submitted by MSI Reproductive Choices. Published 2 May 2023. https://committees.parliament.uk/writtenevidence/120307/pdf/
41. Written evidence submitted by IPPF. Published 2 May 2023. https://committees.parliament.uk/writtenevidence/120306/pdf/
42. WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division (2019). Trends in maternal mortality 2000 to 2017.
43. FCDO (2021). Ending the Preventable Deaths of Mothers, Babies and Children by 2030: Approach Paper. https://www.gov.uk/government/publications/ending-preventable-deaths-of-mothers-babies-and-children-by-2030
44. FCDO (2021). Health Systems Strengthening for Global Health Security and Universal Health Coverage. https://www.gov.uk/government/publications/health-systems-strengthening-for-global-health-security-and-universal-health-coverage
45. GOV.UK. (2022, Oct 19). We must respect the bodily autonomy of women and girls throughout their lives: Cross-regional joint statement at the UN Third Committee. https://www.gov.uk/government/speeches/we-must-respect-the-bodily-autonomy-of-women-and-girls-throughout-their-lives-cross-regional-joint-statement-at-the-un-third-committee
46. GOV.UK (2022, Nov 25). Foreign Secretary announces critical practical support for Ukraine as winter sets in. Press release. https://www.gov.uk/government/news/foreign-secretary-announces-critical-practical-support-for-ukraine-as-winter-sets-in
47. Email correspondence between the House of Commons International Development Committee/House of Lords International Relations and Defence Committee and the FCDO. https://committees.parliament.uk/publications/9161/documents/159656/default/
48. UK Parliament (2022, Dec 13). Reducing the UK’s aid spend in 2021 and 2022. Research Briefing, House of Commons Library. https://commonslibrary.parliament.uk/research-briefings/cbp-9224/
49. FCDO (2023). Statistics on International Development: Provisional UK Aid Spend 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1148898/Statistics-on-International-Development-Provisional-UK-Aid-Spend-2022.pdf
50. FCDO (2023). International Women and Girls Strategy 2023–2030. https://www.gov.uk/government/publications/international-women-and-girls-strategy-2023-to-2030
51. Ibid.
52. GOV.UK (2023, March 8). UK launches new global Women and Girls Strategy on International Women’s Day. Press release. https://www.gov.uk/government/news/uk-launches-new-global-women-and-girls-strategy-on-international-womens-day
53. MSI Reproductive Choices (2023, Feb 2). MSI Senegal meets the UK Minister for Development, Andrew Mitchell. https://www.msichoices.org/news-and-insights/news/2023/2/msi-senegal-meets-the-uk-minister-for-development-andrew-mitchell
54. UK Parliament (2022, May 26). UN Population Fund. Question for Foreign, Commonwealth and Development Office, UIN 9954. https://questions-statements.parliament.uk/written-questions/detail/2022-05-26/9954
55. UNFPA (n.d.). Donor contributions: United Kingdom of Great Britain and Northern Ireland. https://www.unfpa.org/donor/united-kingdom-great-britain-and-northern-ireland
56. DSW and European Parliamentary Forum for Sexual & Reproductive Rights (n.d.). Donors Delivering for SRHR: Report 2021. Tracking OECD Donor Funding for Sexual and Reproductive Health and Rights. https://donorsdelivering.report/wp-content/uploads/2021/09/DD_Report_2021.pdf
57. UNFPA state of the world’s population 2022 (2022). Seeing the Unseen: The case for action in the neglected case of unintended pregnancy. https://eeca.unfpa.org/sites/default/files/pub-pdf/en_swp22_report_0_2.pdf
58. PMNCH (2023, May 3). Why sexual and reproductive health and rights are essential for universal health coverage. https://pmnch.who.int/resources/publications/m/item/why-sexual-and-reproductive-health-and-rights-are-essential-for-universal-health-coverage
59. Sully E.A. et al. (2020). Adding It Up: Investing in Sexual and Reproductive Health 2019 New York: Guttmacher Institute, p.5. https://www.guttmacher.org/sites/default/files/report_pdf/adding-it-up-investing-in-sexual-reproductive-health-2019.pdf
60. PMNCH (2023, May 3). Why sexual and reproductive health rights are essential for universal health coverage. https://pmnch.who.int/resources/publications/m/item/why-sexual-and-reproductive-health-and-rights-are-essential-for-universal-health-coverage
61. World Health Organization (2023). Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. https://www.who.int/publications/i/item/9789240068759
62. Guttmacher Institute (2020, July 23). New Estimates Show Worldwide Decrease in Unintended Pregnancies. News release. https://www.guttmacher.org/news-release/2020/new-estimates-show-worldwide-decrease-unintended-pregnancies
63. UNAIDS (n.d.). Global HIV & AIDS statistics – Fact sheet. https://www.unaids.org/en/resources/fact-sheet
64. UN (n.d.). SDG 5 Gender Equality: Achieve gender equality and empower all women and girls. https://unstats.un.org/sdgs/report/2022/goal-05/
65. Guttmacher Institute (2021, Feb 24). A Time for Change: Advancing Sexual and Reproductive Health and Rights in a New Global Era. Guttmacher Policy Review Vol 24. https://www.guttmacher.org/gpr/2021/02/time-change-advancing-sexual-and-reproductive-health-and-rights-new-global-era
66. Institute for Heath Metrics and Evaluation (n.d.). GBD Compare. https://vizhub.healthdata.org/gbd-compare/
67. Starrs, A.M. et al. (2018). Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. The Lancet, Vol. 391, Issue 10140, 2642–2692. https://doi.org/10.1016/S0140-6736(18)30293-9
68. Guttmacher Institute (2022, March). Unintended Pregnancy and Abortion Worldwide. Fact Sheet https://www.guttmacher.org/fact-sheet/induced-abortion-worldwide#
69. UNAIDS (n.d.). Global HIV & AIDS statistics – Fact sheet. https://www.unaids.org/en/resources/fact-sheet
70. World Health Organization (2022). Abortion care guideline. https://www.who.int/publications/i/item/9789240039483
71. World Health Organization (2022). Abortion care guideline. https://www.who.int/publications/i/item/9789240039483, 2
72. World Health Organization (2019, Nov 11). Preventing unsafe abortion: Evidence Brief. https://www.who.int/publications/i/item/WHO-RHR-19.21
73. World Health Organization (2022). Abortion care guideline. https://www.who.int/publications/i/item/9789240039483, 2
74. Haakenstad A. et al. (2019). Measuring contraceptive method mix, prevalence, and demand satisfied by age and marital status in 204 countries and territories, 1970–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, Vol. 400, Issue 10348, 295–327. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)00936-9/fulltext
75. Lavender T., Wakasiaka S. and Khisa W. (2022). A Multidisciplinary Approach to Obstetric Fistula in Africa: Public Health, Sociological, and Medical Perspectives. In: Drew, L.B., Ruder, B., Schwartz, D.A. (eds) A Multidisciplinary Approach to Obstetric Fistula in Africa. Global Maternal and Child Health. Springer, Cham. https://doi.org/10.1007/978-3-031-06314-5_6
76. World Health Organization. (2018, Feb 19). Obstetric fistula. https://www.who.int/features/factfiles/obstetric_fistula/en/
77. Mishra G.D., Anderson D., Schoenaker D.A.J.M., Adami H.O., Avis N.E., Brown D. et al. (2013, Mar 1). InterLACE: A new International Collaboration for a Life-course Approach to Women’s Reproductive Health and Chronic Disease Events. Maturitas [Internet]. [cited 2022 Aug 4];74(3):235–40. Available from: http://www.maturitas.org/article/S0378512212004112/fulltext
78. Global Burden of Disease Collaborative Network. (2020). Global Burden of Disease Study 2019 (GBD 2019) Results. https://vizhub.healthdata.org/gbd-results/
79. Ibid.
80. Kristiansen M.B., Shayo B.C., Philemon R., Khan K.S., Rasch V. and Linde D.S. (2021). Medical management of induced and incomplete first-trimester abortion by non-physicians in low- and middle-income countries: A systematic review and meta-analysis of randomized controlled trials. Acta Obstet Gynecol Scand, 100:718–726. https://doi.org/10.1111/aogs.14134
81. PMNCH (2023, May 3). Why sexual and reproductive health rights are essential for universal health coverage. https://pmnch.who.int/resources/publications/m/item/why-sexual-and-reproductive-health-and-rights-are-essential-for-universal-health-coverage
82. World Health Organization (2018). Public spending on health: a closer look at global trends. Geneva: WHO. https://apps.who.int/iris/bitstream/handle/10665/276728/WHO-HIS-HGF-HF-WorkingPaper-18.3-eng.pdf
83. PMNCH (2023, May 3). Why sexual and reproductive health rights are essential for universal health coverage. https://pmnch.who.int/resources/publications/m/item/why-sexual-and-reproductive-health-and-rights-are-essential-for-universal-health-coverage
84. Coulson J., Sharma V. and Wen H. (2023). Understanding the global dynamics of continuing unmet need for family planning and unintended pregnancy. China Popul Dev Stud. 2023; 7(1):1-14. doi: 10.1007/s42379-023-00130-7. Epub 2023 Apr 5. PMID: 37193368; PMCID: PMC10075166.
85. United Nations Department of Economic and Social Affairs, Population Division (2022). World Family Planning 2022: Meeting the changing needs for family planning: Contraceptive use by age and method. UN DESA/POP/2022/TR/NO. 4. https://desapublications.un.org/file/1083/download#:~:text=The%20number%20of%20modern%20contraceptive,unmet%20need%20for%20family%20planning.
86. World Health Organization (2008). Task shifting : rational redistribution of tasks among health workforce teams : global recommendations and guidelines. https://apps.who.int/iris/handle/10665/43821
87. World Health Organization (2018). Task sharing to improve access to Family Planning/Contraception. Summary brief. https://www.who.int/publications/i/item/WHO-RHR-17.20
88. FP2020 (n.d.). The Arc of Progress 2019–2020. http://progress.familyplanning2020.org/sites/default/files/FP2020_ProgressReport2020_WEB.pdf
89. Polus S., Lewin S., Glenton C. et al. (2015). Optimizing the delivery of contraceptives in low- and middle-income countries through task shifting: a systematic review of effectiveness and safety. Reprod Health 2015: 12, 27. https://doi.org/10.1186/s12978-015-0002-2
90. Haakenstad A. et al. (2019). Measuring contraceptive method mix, prevalence, and demand satisfied by age and marital status in 204 countries and territories, 1970–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, Vol. 400, Issue 10348, 295–327. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)00936-9/fulltext
91. Ibid.
92. Sully E.A. et al. (2020). Adding It Up: Investing in Sexual and Reproductive Health 2019. New York: Guttmacher Institute, p.12. https://www.guttmacher.org/sites/default/files/report_pdf/adding-it-up-investing-in-sexual-reproductive-health-2019.pdf
93. IPPF (n.d.). About WISH: Leaving no one behind. https://www.ippf.org/about-wish#
94. World Health Organization (2022). Abortion care guideline. https://www.who.int/publications/i/item/9789240039483
95. Ibid. Chapter 1. Introduction: An enabling environment for comprehensive abortion care (1.3). https://srhr.org/abortioncare/chapter-1/an-enabling-environment-for-comprehensive-abortion-care/
96. DeNicola N. et al. (2020). Telehealth Interventions to Improve Obstetric and Gynecologic Health Outcomes: A Systematic Review. Obstetrics and gynecology, 135(2), 371–382. https://doi.org/10.1097/AOG.0000000000003646
97. World Health Organization (2020). WHO recommendations on self-care interventions self-management of medical abortion. https://apps.who.int/iris/bitstream/handle/10665/332334/WHO-SRH-20.11-eng.pdf?ua=1
98. Plesons M., Patkar A., Babb J. et al. (2021). The state of adolescent menstrual health in low- and middle-income countries and suggestions for future action and research. Reprod Health 18, 31. https://doi.org/10.1186/s12978-021-01082-2
99. World Health Organization (2022). Cervical cancer. Fact sheet. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
100. Sully E.A. et al. (2020). Adding It Up: Investing in Sexual and Reproductive Health 2019. New York: Guttmacher Institute. https://www.guttmacher.org/sites/default/files/report_pdf/adding-it-up-investing-in-sexual-reproductive-health-2019.pdf
101. Wirtz C., Mohamed Y., Engel D., Sidibe A., Holloway M., Bloem P., Kumar S., Brotherton J., Reis V. and Morgan C. (2022). Integrating HPV vaccination programs with enhanced cervical cancer screening and treatment, a systematic review. Vaccine. 2022 Mar 31;40:A116-23.
102. World Health Organization (2020). Global strategy to accelerate the elimination of cervical cancer as a public health problem. Geneva: WHO. Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/publications/i/item/9789240014107
103. Ibid.
104. Ibid.
105. Akumbom A.M., Lee J.J., Reynolds N.R., Thayer W., Wang J. and Slade E. (2022). Cost and effectiveness of HPV vaccine delivery strategies: A systematic review. Prev Med Rep. 2022;26:101734. doi:10.1016/j.pmedr.2022.101734
106. Kunckler M., Schumacher F., Kenfack B., Catarino R., Viviano M., Tincho E., Tebeu P.M., Temogne L., Vassilakos P. and Petignat P. (2017). Cervical cancer screening in a low‐resource setting: a pilot study on an HPV‐based screen‐and‐treat approach. Cancer medicine. 2017 Jul; 6(7):1752–61.
107. Fokom Domgue J., Futuh B., Ngalla C., Kakute P., Manjuh F., Manga S., Nulah K., Welty E., Schmeler K. and Welty T. (2020). Feasibility of a community‐based cervical cancer screening with ‘test and treat’ strategy using self‐sample for an HPV test: Experience from rural Cameroon, Africa. International journal of cancer. 2020 Jul 1;147(1):128–38.
108. Joint United Nations Programme on HIV/AIDS (2017). UNAIDS Reference Data 2017. Geneva: UNAIDS. Available from: http://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf. Accessed 14 Dec 2018 [Ref list]
109. Smith M.L., Bergeron C.D., Goltz H.H., Coffey T. and Boolani A. (2020). Sexually Transmitted Infection Knowledge among Older Adults: Psychometrics and Test-Retest Reliability. Int J Environ Res Public Health. 2020 Apr 3;17(7):2462. doi: 10.3390/ijerph17072462. PMID: 32260298; PMCID: PMC7177870
110. Coulson J., Sharma V. and Wen H. (2023). Understanding the global dynamics of continuing unmet need for family planning and unintended pregnancy. China Popul Dev Stud. 2023;7(1):1-14. doi: 10.1007/s42379-023-00130-7. Epub 2023 Apr 5. PMID: 37193368; PMCID: PMC10075166
111. Brandenburger D. and Ambrosino E. (2021). The impact of antenatal syphilis point of care testing on pregnancy outcomes: A systematic review. PLoS ONE 16(3): e0247649. https://doi.org/10.1371/journal.pone.0247649
112. Martin K., Wenlock R., Roper T. et al. (2022). Facilitators and barriers to point-of-care testing for sexually transmitted infections in low- and middle-income countries: a scoping review. BMC Infect Dis 22, 561. https://doi.org/10.1186/s12879-022-07534-9
113. World Health Organization (2023). Mother-to-child transmission of HIV https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/prevention/mother-to-child-transmission-of-hiv#:~:text=Globally%2C%20an%20estimated%201.3%20million,HIV%20become%20pregnant%20each%20year
114. World Health Organization (2023, Jan 31). Female genital mutilation. Fact sheet. https://www.who.int/news-room/fact-sheets/detail/female-genital-mutilation
115. Raassen T.J.I.P., Ngongo C.J. and Mahendeka M.M. (2014). Iatrogenic genitourinary fistula: an 18-year retrospective review of 805 injuries. Int Urogynecol J 2014: 25: 1699–1706. https://pubmed.ncbi.nlm.nih.gov/25062654/
116. Royal College of Obstetricians and Gynaecologists. (n.d.). Essential Obstetric Skills Training. Project period: 2014-2018. https://www.rcog.org.uk/about-us/global-network/centre-for-womens-global-health/essential-obstetric-skills-training/#:~:text=The%20RCOG's%20Essential%20Obstetrics%20Skills,pregnant%2C%20during%20pregnancy%20and%20childbirth.
117. Bello O.O., Morhason-Bello I.O. and Ojengbede O.A. (2020). Nigeria, a high burden state of obstetric fistula: a contextual analysis of key drivers. Pan Afr Med J. 2020 May 18;36:22. doi: 10.11604/pamj.2020.36.22.22204. PMID: 32774599; PMCID: PMC7388624
118. Wall L.L. (2012). Preventing Obstetric Fistulas in Low-Resource Countries: Insights From a Haddon Matrix. Obstetrical and Gynecological Survey, Vol. 67, No. 2. http://prd-medweb-cdn.s3.amazonaws.com/documents/1anesthesiology/files/Article%201.pdf
119. UNESCO, Joint United Nations Programme on HIV/AIDS, UNFPA, United Nations Children’s Fund, United Nations Entity for Gender Equality and the Empowerment of Women and WHO (2018). International technical guidance on sexuality education: an evidence-informed approach. https://unesdoc.unesco.org/ark:/48223/pf0000260770
120. Wall L.L. (2012). Overcoming phase 1 delays: the critical component of obstetric fistula prevention programs in resource-poor countries. BMC Pregnancy Childbirth 12, 68. https://doi.org/10.1186/1471-2393-12-68. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/1471-2393-12-68
121. Plan International (2020). Comprehensive Sexuality Education Programme Standards. https://plan-international.org/publications/comprehensive-sexuality-education-programme-standards/
122. Ruder B. and Emasu A. (2022). The Promise and Neglect of Follow-up Care in Obstetric Fistula Treatment in Uganda. 2022 Jan 1. In: Wallace L.J., MacDonald M.E. and Storeng K.T. (eds). Anthropologies of Global Maternal and Reproductive Health: From Policy Spaces to Sites of Practice [Internet]. Cham (CH): Springer. Chapter 3. Available from: https://www.ncbi.nlm.nih.gov/books/NBK584053/ doi: 10.1007/978-3-030-84514-8_3
123. Slinger G. and Trautvetter L. (2020). Addressing the fistula treatment gap and rising to the 2030 challenge. Int J Gynaecol Obstet. 2020 Jan;148 Suppl 1(Suppl 1):9-15. doi: 10.1002/ijgo.13033. PMID: 31943185; PMCID: PMC7004198
124. Ibid.
125. FIGO (n.d.). Fistula Surgery Training Initiative. https://www.figo.org/what-we-do/obstetric-fistula/fistula-surgery-training-initiative