This International Women's Day we want to focus on gender bias within the world of academia and research. In the UK, fewer than a third (28%) of professors are female, while in 2019 it was reported that there are as few as 25 Black female professors in the UK.
In the world of women’s health, the limited number of female professors in research is almost certainly a contributing factor as to why there is such a gender data gap.
We have interviewed a number of incredible women doing research in women’s health, and we are delighted to provide a platform for their discoveries and ideas to be shared.

As a doctor working in obstetrics and gynaecology (O&G), I realised that conventional management of sexual difficulties of women was sadly lacking and appeared to consist of only laparoscopy - a surgical diagnostic procedure used to examine the organs inside the abdomen - to exclude endometriosis and then discharge of patients where this was normal. I trained concurrently in psychosexual medicine with the Institute of Psychosexual Medicine (IPM) at the same time as I qualified in O&G in 2000 and gained membership of the IPM in 2006. I was the Chair of the institute from 2010–2015.
I worked with health broadcaster and writer Dr Catherine Hood and all the professional bodies helping people with sexual difficulties, to set up a working group and establish a validated tool to look at outcome measures in psychosexual medicine. This was so that we can demonstrate the benefits of psychosexual therapy to patients. Currently, I’m involved in three projects in my trust that I hope will lead to a national change in guidance for sexual pain disorders, gynaecological and bladder cancers and sexual difficulties. I’m also part of a national working group for tocophobia, which is a pathological fear of pregnancy. I’m currently writing a book on sexual difficulties for all healthcare professionals to change consultation skills to better help their patients.
I really hope to change training for gynaecologists in sexual difficulties so that we can all feel confident talking to patients about sex and refer on if necessary. I would like to reduce negative laparoscopy rates in women with sexual pain disorders. This will improve patient care, reduce risk and cost to the NHS. Most women think that gynaecologists are the first port of call for sexual problems but we aren’t currently equipping medical students, doctors and allied healthcare professionals to manage this. Even though we know 7.4% of women are struggling and rates of sexual problems start escalating at the start of sexual activity and during the menopause by more than a third.
There is not just a data gap but a huge gap in the care given to women who have sexual difficulties. Women feel they don’t get the support they need. Sexual problems destroy their lives, they lose partners and often their work and mental health suffer. Pelvic cancers cause sexual problems and there is practically no data or resources available. I’m really hopeful that we can change services nationally to help women.
I caught the research bug as a research fellow in 2001. I looked at mother to embryo viral transmission risk in assisted conception in HIV positive women. I found a group of women with no voice and found myself challenging stigmas around their care across all levels including in medicine. Collecting data and improving patient care has become my passion. I like to give patients a voice in stigmatised health conditions. My psychosexual patients are often seen by multiple health care professionals before me and feel completely broken and unfixable. There is no better feeling than getting them back to normal life after multiple years of suffering. Incredible job satisfaction! And I meet amazing and inspiring women-both patients and colleagues.

I was always attracted to O&G as it was a blend of medicine and surgery as opposed to one or the other. Embarking on research in the area of my clinical expertise was a natural next step.
Since the very beginning, it has been early detection of ovarian cancer and identifying and managing women at increased risk of this disease.
What I am most proud of is that through our multicentre trials we were able to bring together the whole ovarian cancer community. We carried out one of the largest randomised controlled trials in the world and the trial management platforms we built ensured safe and timely screening of the women. The trials have generated rich data which is invaluable to our research, and the people involved in the trials will be followed over time with continuous or repeated monitoring of risk factors or health outcomes, or both, which makes possible early detection research into nearly all cancers of older women.
At the same time, we have for the first time shown that through screening we can detect ovarian cancers earlier, although to date we have not been able to impact on mortality. While we await the results of long term follow-up of the UK Collaborative Trial of Ovarian Cancer Screening, we are working with researchers across the globe exploring new biomarkers and technologies to detect ovarian cancer earlier.
Working in research is hugely rewarding – it expands the reach of what you can achieve for your patients. You get to work and think with a multidisciplinary team of inspiring and brilliant researchers and intellectually it stretches you beyond your wildest dreams.



As an obstetrician, the thrill you feel being there at a birth never goes. It is really rewarding. With research, it’s so exciting discovering things that no one else has discovered before. We’re all putting tiny pieces of the jigsaw together but overall, it’s really meaningful and purposeful that can have a positive effect on people’s lives.
My research has, both in the UK and internationally, focused on understanding the causes of preterm birth and stillbirth (including pregnancy stressors such as obesity) and developing and testing strategies to reduce the devastating effects of these conditions on women and their babies. Although we are still a long way from finding the cure for (or the cause of) preterm labour, we are making progress, and hopefully one day this will no longer be a problem condition. One of the most exciting things I have been involved in recently is a global health project on preterm birth prevention. Working with colleagues in the UK, Malawi and Zambia, and a very talented PhD student, we are training midwives and other healthcare professionals to scan women so they can determine how many weeks pregnant they are. This will enable treatment (including prenatal steroids) to be targeted to the right women, enabling health care professionals in low-income settings to better support women during pregnancy and help to reduce the risk of stillbirth and the adverse outcomes of preterm birth.
I entered this field because to me it felt really important. You have a real ability to make a big difference to people’s lives, and there are so many things we still don’t know. One of the things I have learned is how much faster we can progress with team work. When groups of people work together on a goal, they can really pool their expertise and resources, and advance much more quickly. All the things that I have been most proud of in ‘my’ own research have very much been team efforts, and it has been a real privilege to work with others.
There are huge data gaps in women’s health. In pregnancy for example, we still don’t really know what starts off labour at term, let alone preterm labour. We have some idea about the short term impacts that many of the drugs we use in pregnancy have, but there are still a lot of data gaps about long term effects. And we need to know a lot more about the impact of commonly used drugs in pregnant women. The COVID-19 vaccine has been a good example of this ‘missing data’ – it is only now that we are starting to collect information on the impact of vaccination with research studies and that pregnant women are starting to be included in COVID-19 vaccine studies.
From my experience, research has been a great career because is incredibly rewarding and great fun. Many women have lots of good ideas about how to make things better for patients, and how we can understand health and disease better. I believe that women work really well in teams both as team leaders and as team members, so they are very well suited to the ‘team effort’ which is required for almost all good research these days. As a researcher, every day truly is different, and there is a real opportunity to follow the ideas that you are interested in, as long as you can persuade other people that they are interesting too!



In my midwifery clinical practice, I used to work as part of a high-risk maternal medicine team where we looked after women with various chronic conditions. Understanding the evidence was always key to giving as much personalised care as possible. I wanted to be able to explain even deeper how research impacted the guidelines that were used, and the care women and birthing people received. And to do that, I needed to understand the biomedical side of some of the pathology I saw. So, for my role as a research midwife, I worked at Imperial College London in the Women's Health Research Centre, in studies that looked at pre-eclampsia, obstetric cholestasis and also some kidney-related conditions. This helped me talk about the conditions to women and birthing people and my work colleagues in ways that made translation research, which applies findings from basic science to enhance human health and well-being, a tangible goal.
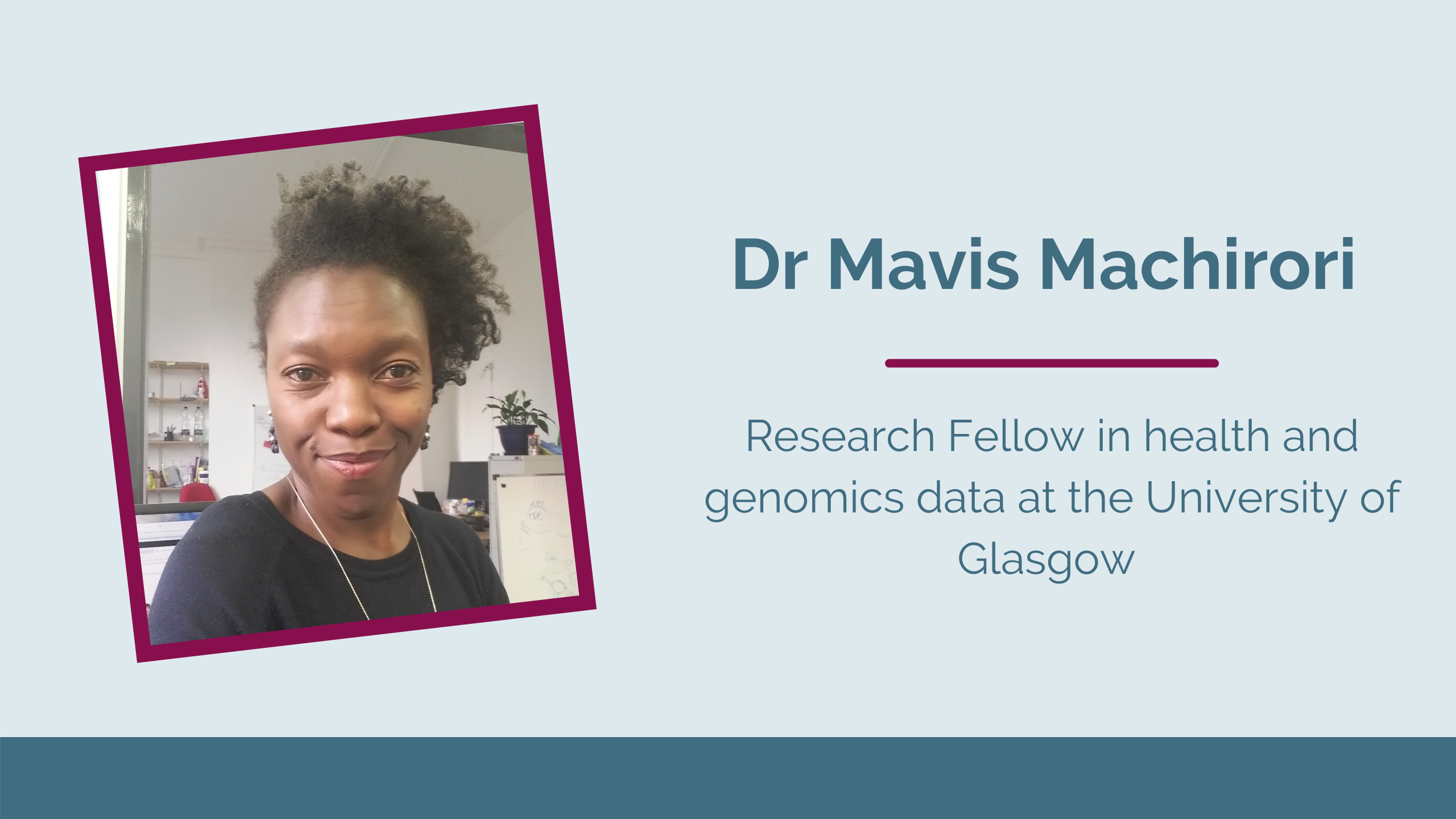
I have since moved from that role, and I now, through a variety of pathways, work in research that looks at how we govern and use health, genomic and other personal data for research purposes. In this role, I observe decision-making around data access, the building of large research groups and consider some of the ethical and societal issues that may arise in that space. I also consider how public engagement can provide meaningful outputs and impact from research, so that we do not do research for its own sake. I am also interested in how these practices impact the inequalities we see in health.

One of the biggest issues, in my opinion, is the lack of voice that those impacted by research have. This can be across demographics such as gender, income or geographical levels. And when we look at additional dimensions such as ethnicity and culture, we see that some characteristics put people at a disadvantage. By understanding the disproportionate impact of research on various communities, I can then highlight areas that need improving - and sometimes will respond to calls for evidence from Parliament, or through policy reports.
There definitely is a data gap. A lot of times, the data we record on people is put into pre-set categories, and so if anything does not fit that category, it may get discarded or written as sub-text. That sub-text may not be analysed which limits what we can then know about people. We already know that the role of clinical trials is important, yet, aside from pregnant women, minority communities are being under-represented in research, there is also unbalanced research between high income and low-middle income countries. So, if you are a woman who comes from all those categories, you are even less likely to have information about you known. This is then worsened by the everyday inequalities that women face, in trying to make themselves heard against a male norm.

We have such an amazing opportunity to steer research in the direction that works for us. We can ask questions that impact us in direct ways, based on our actual lived experiences. And we can re-write the books and be more visible in both biomedical and social research. Only we can define normal for us. There is so much space to accommodate many more women in research, so come claim that space!

When I started work on abortion in 2001 there was very little information and knowledge about the issue. In fact, abortion was a taboo subject in Africa. I realised very quickly that statistical evidence about the numbers and which women were dying or being maimed would be necessary to engage with policymakers at country and regional levels.
Everybody wanted the evidence on how many women were dying especially in their own country/jurisdiction and which category of women were dying. This meant we had to design research that would generate those answers to help provide the evidence base for work in access to safe abortion.
The research work that I commissioned was aimed at providing answers on the issue of unsafe abortion. The problem was that abortion statistics were not always or well recorded so it was not easy to establish cases of abortion from available records and documentation. We also conducted strategic assessments using the World Health Organization (WHO) methodology. This involved engaging relevant in-country partners like ministries of health and other ministries, as well as policymakers and individuals from national and community level, to answer predetermined questions and come up with recommendations about issues of reproductive health and abortion. In some instances, it was necessary to do cost studies to show that it was so much cheaper to provide safe abortions than to treat complications arising from unsafe abortion, which could even cause the death of women.
Most of the research I commissioned, and/or participated in, established facts or answers for advocacy or showed the way for moving forward on issues of women’s health and unsafe abortion. We also undertook action research to pave the way for work in this novel and difficult terrain of abortion. With the available research answers we were able to mount a credible and powerful advocacy program at regional, sub-regional and country levels. In several countries, the results and evidence led to policy changes in favour of access to safe abortion.
The very first research activity on unsafe abortion I was involved in was in the mid-1990s was called ‘The Mothercare Study’. The aim was to create evidence in Ghana on the feasibility of training midwives to deliver post-abortion care. The result was positive and emphatic and informed the WHO’s recommendation for midlevel medical professionals to provide abortion care.
There is indeed a gender data gap when it comes to women's health. This is because for the longest time women’s health issues were not considered important or a priority. Women’s health issues were greatly neglected. I believe the two international women’s conferences in the mid-1990s –the International Conference on Population and Development and the Beijing Conference - were very important in bringing out issues relating to women in general and their health, especially their reproductive health.
The problems that face women in many areas of life and health are far from resolved. There is so much more that needs to be unravelled and having more women conduct research on women’s issues amongst other things would be great. We need a great deal of information on the issues that adolescents face and how to deal with these. There is a great need out there!





I trained as a midwife in London and worked in Malawi, Africa, for four years in a public maternity hospital in the ‘80s. During that time, we were a test site for WHO and, in working in a very busy labour ward and having my first two children in that setting, my experiences of how research can improve care and save lives in resource-poor settings inspired me to do research myself when I returned to the UK. Working part-time as a health visitor working with homeless families, I undertook degrees in social science to equip me to move into an academic/research role. I moved into midwifery education as a clinician/educator to lead a new degree programme for midwives. I was fortunate to be awarded a Department of Health PhD Fellowship for nurses and midwives and my PhD in Sociology looked at the implementation of new models of care and the impact on the midwifery workforce. Having a full-time funded fellowship was a game-changer for me (now with three children) and this is why I think this is so important for health professionals to have these opportunities, particularly those with parental responsibilities as many women have.
My research focuses on safety and quality in maternity and perinatal care, and includes birth outcomes in different settings, maternity workforce skill mix, management of escalation of care in acute medical and maternity settings, engagement by patients and families in their own safety, and implementation of open disclosure in perinatal care. Current research is looking at mechanisms and impact of models of midwife continuity of care for women at higher risk of pre-term birth. Also, interventions to reduce inequities in care looking at mechanisms and outcomes for women and babies using linkage of routinely collected clinical data.
I have expertise in a range of health and social research methods from ethnographic and qualitative methods, modelling of national datasets and trials of complex interventions. I lead Cochrane reviews and have experience leading programmes of applied research in safety and quality in collaboration with key stakeholders and the public.

I have trained in implementation science and work with local, regional and national policy bodies in the UK regarding translation of research evidence into policy and practice, for example, NHS England Continuity of Midwifery care expert group, NICE Implementation Strategy Group, NHSE London Clinical Leadership group to reduce maternal and perinatal mortality and morbidity. At a global level I have served as a ministerial appointed expert on the review of Irish Maternity strategy, co-chaired the ICM Research Committee for 8 years and contributed to international midwifery initiatives such as the Lancet Series on midwifery and caesarean section. My research findings have informed the UK, US, Irish and Australian maternity policies and WHO guidance.
It takes too long between the production of implementable evidence to become policy and practice with the result that women, families and services don’t benefit from this knowledge. There is too much silo working between disciplines and approaches. For example, in tackling inequities and inequalities, we need to involve biomedical scientists, epidemiologists, triallists, clinicians, social scientists and public health expertise plus women, family and community voices to have a better understanding of the issues and of what works for whom in what circumstances.
It is crucial to have a diversity of voices in research so we ask the right questions, design the right research and engage with the right people who have an interest in our research. We know that we need to have more women in senior research positions and my role is focused on more midwives having the opportunities than at present.
Working in research is fun, you can be curious and have real world impact.

Research helps to make sense of what we are doing clinically, to improve care and outcomes for pregnant women. Research has given us some answers, but there is much more to understand.
My research focus is particularly on pregnancy hypertension.
Our research is collaborative, both within our group, and with national and international colleagues, and working with patient groups. We try and add to the collective knowledge around pregnancy hypertension, particularly around improving prediction and diagnosis and optimising treatment to reduce the impact of the disease for women and babies. For example, our work has contributed to the introduction of a new test for women with suspected pre-eclampsia, based on placental growth factor measurement, leading to faster diagnosis and reduced complications.
Whilst pregnancy research itself focuses on women, there is a data gap more widely, with many areas of research outside of pregnancy showing biases at design, recruitment and interpretation stages. We can all help by working to get research reported transparently, including gender and ethnicity characteristics, and ensuring that there is equity at all stages of the research pipeline, so that this gap is narrowed.
More recently, I have been working with the RCOG to co-ordinate messaging for clinicians and women around COVID-19 vaccines, pregnancy and fertility. A gap in the data available in this area, and the absence of any clinical trials of COVID-19 vaccines in pregnant women, has meant there we have been working hard to try and get clear messaging to women. This is one example of where a gender data gap is having an impact on the health of women.
My research work is one of the most rewarding aspects of my career, with enormous opportunities to work towards better health for women and their babies.




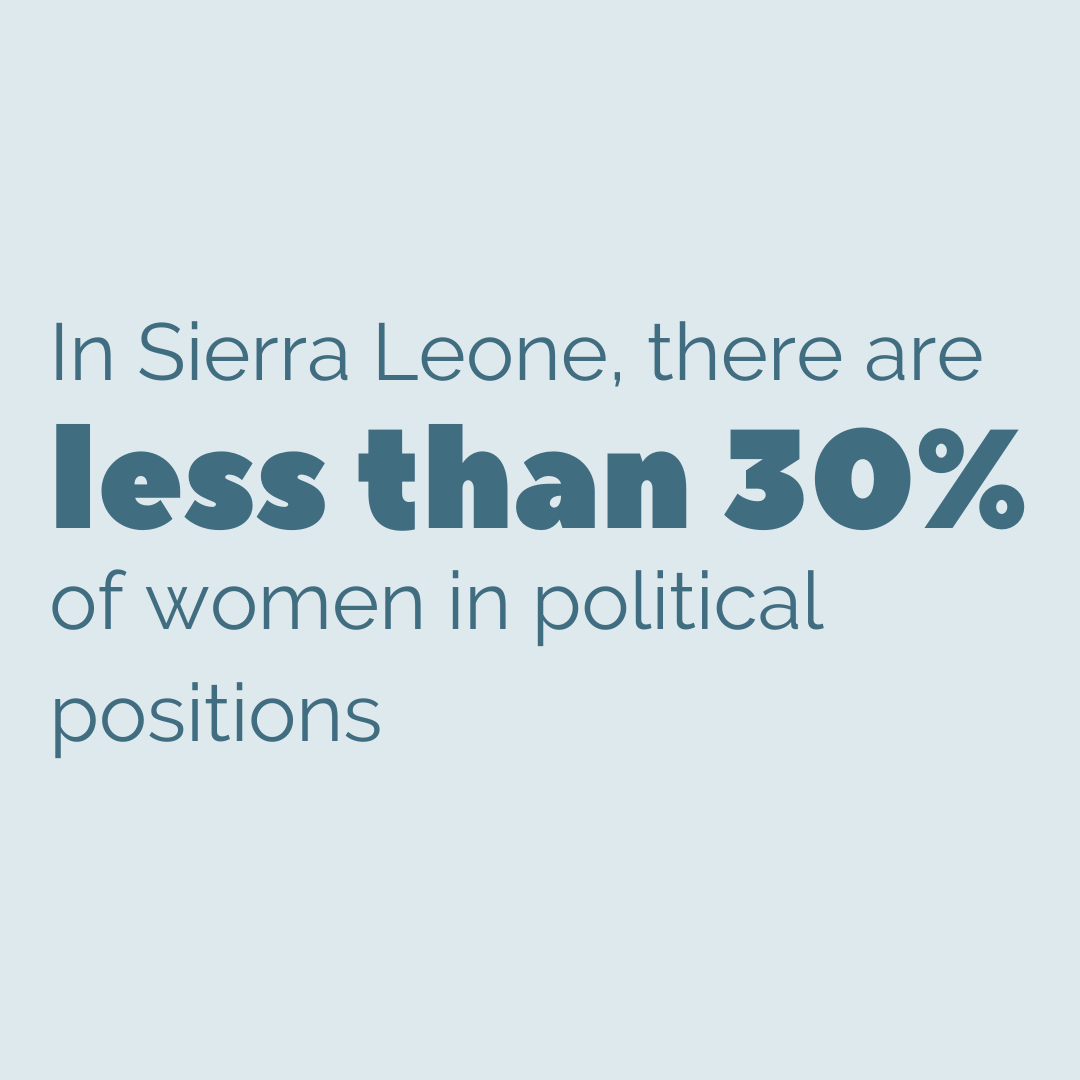
In Sierra Leone, there are less than 30% of women in political positions. Therefore, women are under-represented in spaces where decisions affecting their health, safety and wellbeing are made. This has guided my research focus as I aim to amplify the voices of marginalized women and girls who usually will not be heard. Through our study findings we hope to give decision-makers the information they need to implement impactful and life-changing policies.
My research focus is on women and children’s health with particular attention paid to marginalised groups such as women and girls living in extreme poverty, survivors of human trafficking, commercial sex workers, women and girls living with disabilities and children living within kinship foster arrangements.
Researching the lived experiences of these groups of people is an important part of understanding how laws affect those who are rarely considered when decisions are made. Research outputs are the foundation of evidence-based decision making and I feel my research helps not only policymakers in making the right decisions encompassing the views of everyone living in our communities; but also empowers these communities to know what questions they should be asking and links them to their key stakeholders so they can hold them accountable to their promises.

In Sierra Leone and similar settings, limited data is available when it comes to abortion. Abortion is illegal in Sierra Leone, making an already sensitive topic difficult to study with participants being hesitant in coming forward for fear of persecution and stigma. Researchers may be hesitant to commit technical and financial resources to conduct research whose findings may not be implemented.
The lack of abortion data undermines the importance of providing safe abortion care and makes it easy to ignore the morbidity and mortality associated with unsafe abortions. Inadequate data is also problematic for sexual and reproductive health activists, as well as health professionals, to lobby change-makers to provide affordable safe abortion care to every woman and girl who needs it.
As women we must tell our own stories. We must find the answers to questions important to us and present these findings to those who can improve on our health, safety and wellbeing. As we demand all decisions be made through the gender lens, who better to provide evidence to decision-makers than female researchers? Even though our numbers are still limited in decision making spaces, we should provide the data needed to make decisions benefiting us.